It feels like there’s always something new popping up in medicine, and cardiac ablation is no different. Boston Scientific has a new system called FARAPULSE that’s getting a lot of attention. It uses a different method than what doctors have been using for years to treat things like atrial fibrillation. This new approach, called pulsed field ablation (PFA), seems to have some pretty good benefits, especially when it comes to safety. Let’s break down what this means and why it’s being called a potential game-changer.
Key Takeaways
- Boston Scientific’s FARAPULSE PFA system uses pulsed field ablation, a non-thermal method to treat cardiac arrhythmias like atrial fibrillation.
- PFA works by using electrical fields to create tiny holes in cell membranes, specifically targeting heart cells while sparing nearby structures.
- Clinical trials, including the ADVANTAGE AF and ADVENT studies, show the boston scientific pfa system is effective and has a good safety record compared to older methods.
- The system has received FDA approval for treating persistent atrial fibrillation, opening doors for more patients and potential use in redo procedures.
- While PFA shows promise for faster procedures and fewer complications, ongoing research and cost analyses are important for its widespread adoption.
Boston Scientific’s FARAPULSE PFA System: A Paradigm Shift
It feels like just yesterday we were talking about the latest advancements in cardiac ablation, and now, here we are, on the cusp of something truly new with pulsed-field ablation (PFA). Boston Scientific’s FARAPULSE PFA System is really shaking things up, moving us away from the older methods and into a more precise, safer way to treat atrial fibrillation (AF).
Understanding Pulsed Field Ablation Technology
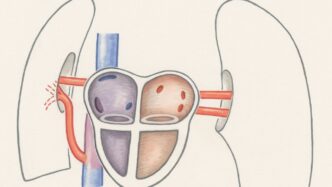
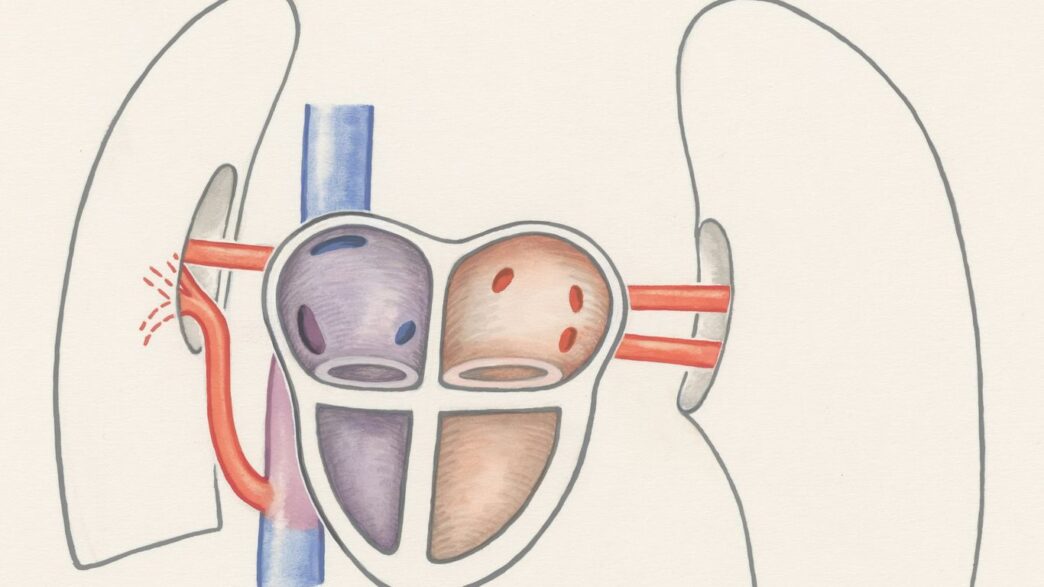
So, what exactly is PFA? Instead of using heat or cold to create lesions in the heart tissue, PFA uses short, high-voltage electrical pulses. Think of it like this: these pulses create tiny pores in the cell membranes of the heart muscle cells. The key here is that these pulses are designed to be much more selective, targeting the heart cells while leaving nearby structures, like the esophagus and nerves, largely unharmed. This is a big deal because damaging those nearby parts has been a major concern with older ablation techniques.
The Emergence of Irreversible Electroporation in Cardiac Ablation
PFA is a form of irreversible electroporation (IRE). The idea behind IRE is to create permanent cell death by disrupting the cell membrane. The FARAPULSE system uses specific electrical field parameters to achieve this effect in cardiac tissue. It’s a nonthermal method, which is a pretty significant departure from radiofrequency (RF) or cryoablation. This nonthermal aspect is what really sets it apart in terms of safety for surrounding tissues.
Mechanism of Pulsed Field Ablation Explained
When the FARAPULSE system delivers its pulses, it creates an electrical field around the catheter tip. This field causes the cell membranes of the cardiomyocytes to form pores. If the pulses are strong enough and delivered in the right way, these pores don’t close back up, leading to cell death. The magic is in the timing and intensity of these pulses – they’re short enough and specific enough to affect the heart cells without causing thermal damage to the esophagus or nerves. It’s a delicate balance, but one that seems to be working really well based on early results.
- Selective Cell Death: The primary mechanism targets cardiac myocytes, minimizing damage to adjacent structures.
- Nonthermal Process: Unlike RF or cryoablation, PFA does not rely on heat or cold, reducing risks like esophageal injury or phrenic nerve damage.
- Rapid Lesion Formation: PFA can create effective lesions quickly, potentially leading to shorter procedure times.
The shift towards PFA technology represents a significant step forward in cardiac ablation. Its ability to precisely target cardiac tissue while sparing critical nearby structures offers a compelling safety advantage, potentially broadening the applicability of ablation procedures and improving patient outcomes.
Clinical Evidence Supporting FARAPULSE PFA
So, what’s the actual proof that this FARAPULSE PFA system is as good as they say? Well, a bunch of studies have been looking into it, and the results are pretty encouraging. It seems like this technology is really shaking things up in how we treat atrial fibrillation (AF).
ADVANTAGE AF Trial Results
The ADVANTAGE AF trial was a big one, focusing specifically on how well the FARAPULSE system works for persistent AF. It was a single-arm study, meaning everyone got the PFA treatment. The main goal was to see if it could effectively isolate the pulmonary veins, which is key to stopping AF. Early findings showed that the system achieved pulmonary vein isolation in a very high percentage of patients. This is a good sign that it’s doing its job.
ADVENT Trial Findings on Safety and Efficacy
Then there was the ADVENT trial. This one was a bit different because it was a randomized clinical trial, comparing PFA directly against traditional thermal ablation methods (like radiofrequency or cryoablation). They looked at over 300 patients across multiple centers in the US. The big takeaway here? The FARAPULSE PFA system met the mark for both safety and how well it worked, showing it’s just as good as the older methods, and in some ways, even better.
Here’s a quick look at what the ADVENT trial and others have suggested:
- High Success Rate: Pulmonary vein isolation was achieved in nearly all patients.
- Low Complication Rate: Major issues like stroke or heart problems were rare.
- Faster Procedures: Patients spent less time in the operating room compared to cryoablation or RF ablation.
- Durability: After a year, a good number of patients remained free from AF, even those with persistent forms.
The evidence is building up, showing that PFA isn’t just a theoretical concept; it’s proving its worth in real-world patient care. The ability to achieve effective ablation with a better safety profile is a significant step forward.
Real-World Data from MANIFEST-17K Survey
Beyond the controlled trials, there’s also real-world data being collected. The MANIFEST-17K survey, for instance, gathered information from a large number of patients treated with FARAPULSE. This kind of data helps us understand how the system performs outside of strict trial conditions, looking at things like procedure times, success rates, and any adverse events in a broader patient population. The initial reports from these kinds of surveys often mirror the trial findings, reinforcing the system’s effectiveness and safety in everyday practice.
FARAPULSE PFA: Safety and Efficacy Compared to Thermal Ablation
Reduced Risk to Adjacent Structures
One of the big selling points for the FARAPULSE PFA system is how it handles nearby tissues. Unlike older methods that use heat (like radiofrequency) or cold (cryoablation), PFA uses short, intense electrical pulses. This is called irreversible electroporation. The idea is that heart muscle cells are more sensitive to these pulses than other structures. This means the system can zap the problematic heart tissue causing atrial fibrillation without causing as much harm to things like the esophagus, phrenic nerve, or blood vessels. It’s like being able to target just the weeds in your garden without damaging the flowers. This selective approach could mean fewer scary side effects that sometimes come with traditional ablation.
Lower Incidence of Major Complications
When you look at the numbers from studies, the FARAPULSE system seems to be doing pretty well on the safety front. For instance, the MANIFEST-17K survey, which looked at over 17,000 patients treated with the FARAPULSE system, showed a really low rate of major problems – less than 1%. Most of the issues that did pop up were things like pericardial tamponade (fluid around the heart), stroke, or coronary artery spasm. While these are serious, the overall incidence appears to be lower compared to what’s often seen with thermal ablation techniques. It’s still early days, and more data will keep coming in, but the initial signs suggest a good safety profile.
Faster Procedure Times
Who doesn’t like a quicker procedure? Patients and doctors alike tend to appreciate when things move along efficiently. Reports from clinical trials suggest that procedures using the FARAPULSE PFA system can be faster than those using cryoablation or radiofrequency ablation. This isn’t just about saving time in the operating room; faster procedures can mean less anesthesia, reduced patient discomfort, and potentially lower overall healthcare costs. It’s a win-win situation if it holds up across the board.
The shift towards pulsed field ablation, exemplified by systems like FARAPULSE, represents a significant step forward in cardiac ablation. By prioritizing tissue selectivity, the technology aims to maintain high efficacy in treating arrhythmias while markedly reducing the risk of collateral damage to critical surrounding structures. This focus on safety, coupled with procedural efficiency, positions PFA as a potentially transformative option for patients suffering from atrial fibrillation.
Expanding Indications for Boston Scientific’s PFA System
So, Boston Scientific’s FARAPULSE PFA System isn’t just for the most common type of atrial fibrillation anymore. It’s like they’ve figured out how to make it work for more complicated heart rhythm issues too. This is pretty big news because it means more people could potentially benefit from this less invasive approach.
FDA Approval for Persistent Atrial Fibrillation
One of the major steps forward is the FDA giving the green light for the FARAPULSE PFA system to treat persistent atrial fibrillation. This is a tougher form of AF where the heart’s upper chambers have been out of rhythm for a longer time, often a year or more. Before, PFA was mainly used for paroxysmal AF, the kind that comes and goes. Now, with this expanded approval, the system can be used to isolate not just the pulmonary veins but also the posterior wall of the left atrium. This is a significant move because treating persistent AF has historically been more challenging.
Potential for Redo Ablations and Complex Arrhythmias
What’s also really interesting is the potential for using PFA in redo ablations. You know, when a patient has already had an ablation, maybe with older methods, and the AF comes back. These redo procedures can be tricky because there’s already scar tissue from the first attempt. The idea is that PFA’s unique way of targeting cells might be safer and more effective in these situations, especially when dealing with arrhythmias that are located near important structures in the heart. Think about it – if you can get the job done without as much risk to nearby tissues, that’s a win.
Treatment of Drug-Refractory Symptomatic AF
This system is now indicated for patients with symptomatic AF that hasn’t responded well to medications. It’s for those who are still experiencing bothersome symptoms like fatigue or palpitations, even after trying different drugs. The FARAPULSE PFA system offers another option when medications aren’t cutting it. It’s all about giving doctors more tools to help patients get back to a more normal heart rhythm and improve their quality of life. The goal is to provide a treatment that’s both effective and has a good safety record, especially when other options have been exhausted.
Future Directions and Integration of PFA Technology
So, what’s next for pulsed field ablation (PFA) in treating heart rhythm issues? It’s a pretty exciting time, and things are moving fast. We’re seeing a lot of research and development that could really change how we approach these conditions.
Ongoing Clinical Trials and Research
Right now, a bunch of studies are looking into how PFA can be used for more than just the common types of atrial fibrillation (AF). Think about long-standing persistent AF, which is tougher to treat, or even other arrhythmias like ventricular tachycardia. The idea is that PFA’s ability to target heart tissue without harming nearby important structures could make it a safer choice for these more complicated cases. We’re also seeing investigations into using PFA for redo ablations, where scar tissue from previous procedures can make things tricky.
Integration into Clinical Guidelines
As more data comes out showing how well PFA works and how safe it is, you can bet that major heart organizations will start including it in their official treatment recommendations. It makes sense, right? Especially for patients who might be at higher risk with traditional heat-based ablation methods – maybe they have issues with their esophagus, or their phrenic nerve is sensitive, or they’ve had a failed ablation before. PFA could become a go-to option for them.
Technological Advancements in PFA Systems
This technology isn’t standing still. We’re expecting to see improvements in the catheters themselves, the systems that deliver the energy, and how they connect with heart mapping tools. Imagine systems that can show you in real-time if the ablation worked perfectly – that would be a game-changer for accuracy and reducing the need for repeat procedures. They’re also working on making the catheters more flexible and easier to steer, which should make the whole process smoother for doctors and patients alike.
The journey of PFA from a lab concept to a widely used clinical tool has been incredibly quick. This rapid adoption isn’t just about its good safety and effectiveness; it’s also about how fast procedures can be done and how quickly doctors can learn to use it. This efficiency is a big deal in busy cardiac centers.
Here’s a quick look at what’s on the horizon:
- Broader Applications: Moving beyond just pulmonary vein isolation (PVI) to tackle more complex arrhythmias and potentially other heart rhythm disorders.
- Smarter Tools: Development of real-time feedback mechanisms to confirm lesion creation and improve precision.
- Improved Catheter Designs: More flexible, steerable, and potentially multi-electrode catheters for better navigation and coverage.
- Long-Term Data: Continued studies to confirm the durability of PFA lesions and its long-term impact on patient outcomes, like stroke risk.
The Economic Landscape of Pulsed Field Ablation
So, let’s talk about the money side of things with this new Pulsed Field Ablation (PFA) technology. It’s not just about the science and how well it works in the heart; it’s also about how it fits into the bigger financial picture for hospitals and patients. When a new medical device comes out, especially one that’s a bit of a game-changer like PFA, there’s always a lot of figuring out to do regarding costs and benefits.
Comparing Procedural Costs
Right now, PFA systems, including the hardware and the catheters, can be more expensive upfront compared to traditional radiofrequency (RF) or cryoablation tools. Think of it like buying a new, high-tech gadget versus an older, reliable model. The initial investment for PFA equipment is higher. However, the story doesn’t end there. We need to look at the whole procedure, not just the price tag of the device itself.
- Initial Device Costs: PFA catheters and generators tend to have a higher purchase price.
- Procedure Time: Early data suggests PFA procedures might be quicker than some thermal ablations. If procedures are faster, that means more patients can be treated in the same amount of time, potentially increasing throughput and revenue for the hospital.
- Reduced Complication Management: This is a big one. If PFA leads to fewer serious complications, like damage to the esophagus or nerves, then hospitals save money on managing those issues. Think about the costs associated with extended hospital stays, additional treatments, or even legal fees if something goes wrong. The potential for lower complication rates could offset the higher initial device cost over time.
- Resource Utilization: Shorter procedure times and fewer complications can also mean less use of operating room resources, fewer staff hours needed per patient, and potentially shorter recovery periods for patients.
Long-Term Economic Impact of PFA Adoption
Looking down the road, the economic impact of PFA adoption is pretty interesting. While the upfront costs are a hurdle, the long-term savings could be significant. If PFA becomes the go-to method for many atrial fibrillation cases, especially those that are tricky or persistent, its widespread use could drive down costs through economies of scale. Manufacturers might be able to produce the devices more cheaply as demand increases, and hospitals might negotiate better prices.
The shift towards PFA isn’t just about adopting new technology; it’s about rethinking the entire economic model of cardiac ablation. It involves balancing initial capital expenditure against potential savings from reduced complications, shorter procedure times, and improved patient outcomes. As more data becomes available and the technology matures, the economic justification for PFA is likely to become even stronger.
Market Dynamics and Cost Reduction
As more companies enter the PFA market and more clinical trials demonstrate its value, competition will likely increase. This competition is usually good for consumers, meaning hospitals and eventually patients, as it tends to drive prices down. We’re already seeing different PFA systems being developed, each with its own features and cost structure. The more options available, the more likely we are to see price reductions and innovations that make the technology more accessible. It’s a bit of a waiting game, but the trend seems to be moving towards making PFA a more economically viable option for a wider range of healthcare settings. The goal is to make this safer, potentially more effective treatment available to more people without breaking the bank. It’s a complex puzzle, but one that’s definitely worth solving for better patient care.
Looking Ahead with FARAPULSE
So, what does all this mean for treating atrial fibrillation? Basically, the FARAPULSE system seems to be a pretty big deal. It’s showing real promise in making cardiac ablation safer and maybe even quicker. While it’s still early days and more studies are planned, especially for tricky cases like repeat procedures or more complex heart rhythms, the initial results are encouraging. It looks like pulsed field ablation, and specifically the FARAPULSE system, could really change how doctors approach AFib treatment down the road. It’s exciting to see new tech that might offer a better option for patients.