AI in cancer diagnostics is changing the way we find and treat cancer, and 2025 looks like a big year for this technology. It’s not just about reading scans faster—AI is helping doctors spot cancer earlier, sort through mountains of patient data, and even pick out treatments that fit each person better. These tools are popping up in clinics, labs, and even on our phones, making care more personal and more available to everyone. There’s still a lot to figure out, like privacy and making sure it works for everyone, but the progress so far is pretty exciting.
Key Takeaways
- AI in cancer diagnostics is helping doctors catch cancer earlier by finding patterns in scans and health records that people might miss.
- Wearables and non-invasive tech, powered by AI, are making it easier to keep an eye on health and spot warning signs without trips to the hospital.
- AI is speeding up the process of sorting through huge amounts of patient data, which means faster and more accurate results for patients.
- Personalized treatments are becoming a reality, with AI helping match therapies to each person’s unique genes and cancer type.
- As AI tools spread, they’re making cancer care more available in places with fewer resources, but there are still big questions about privacy and fairness.
Revolutionizing Early Cancer Detection with AI in Cancer Diagnostics
Artificial intelligence in cancer diagnostics is changing how fast and accurately we can spot cancer, sometimes before symptoms even start. These smart tools aren’t just for big hospitals; they’re showing up everywhere—at imaging centers, in clinics, and even connecting with devices people can use at home. Let’s look at three ways AI is reshaping early detection.
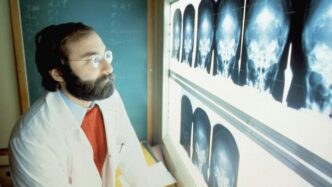
Advanced Imaging Technologies for Early Tumor Identification
AI is making a real difference in analyzing medical scans such as mammograms, CTs, MRIs, and ultrasounds.
- Systems look for patterns on scans that are too subtle or complex for the human eye to notice.
- Faster and more repeatable diagnoses—AI can scan thousands of images in the time it takes a person to read one.
- Machine learning reduces false negatives (missed cancers) and false positives (unnecessary follow-ups).
| Screening Type | Traditional Sensitivity | AI-Assisted Sensitivity |
|---|---|---|
| Breast Mammography | 85% | 90%+ |
| Low-Dose Lung CT | 60-70% | 85%+ |
| Colonoscopy (Polyp) | 25% | 40%+ |
By picking out the smallest, earliest signs of cancer, AI gives patients a better shot at early treatment and improved recovery.
Proactive Risk Prediction Through Big Data Analytics
AI’s ability to handle huge amounts of data—from family history to test results—means it can now help doctors figure out who is at higher risk for certain cancers before any symptoms occur.
- Combines personal health, genetics, lifestyle, and population data to estimate cancer risk.
- Flags high-risk individuals for earlier or more frequent testing.
- Adjusts to new information, updating risk in real time as people’s health changes.
Often, these prediction models encourage people who otherwise wouldn’t get checked out to see their doctor sooner, potentially catching cancer in stages where it’s most treatable.
Integration of Wearables and Non-Invasive Monitoring
Wearable health trackers and home sensors are becoming smarter thanks to AI. These devices quietly collect information—like heart rate, activity levels, or minor changes in routine—and can spot patterns that might signal early warning signs.
- Monitors warning signs outside the clinic, catching changes that could suggest hidden cancers.
- Relieves pressure on health systems by shifting some checks from hospitals to homes.
- Makes it easier for people in remote or underserved areas to access early detection.
List of non-invasive methods supported by AI:
- Smart watches tracking subtle symptoms.
- Blood, saliva, or urine tests done at home and analyzed through cloud-based AI.
- AI-powered imaging apps helping doctors in local clinics review patient data remotely.
The move toward continuous, at-home cancer monitoring is making early detection possible for more people, no matter where they live.
Enhancing Diagnostic Accuracy and Speed with AI in Cancer Diagnostics
AI isn’t just about working faster—it’s about working smarter when it comes to cancer diagnostics. With more complex datasets and increasing patient loads, AI-based tools are now handling many tasks that once took clinicians hours, bringing both accuracy and speed to the forefront of cancer care in 2025. Here’s a look at how these intelligent systems are reshaping the field.
Automated Pattern Recognition in Radiology and Pathology
Gone are the days when radiologists or pathologists solely relied on the naked eye. Smart algorithms comb through thousands of digital scans and biopsies, pointing out patterns that humans can easily miss. AI-powered tools now:
- Spot tiny changes or unusual features on MRIs, CTs, mammograms, and pathology slides
- Help distinguish benign from malignant lesions, often with greater consistency than manual inspection
- Highlight suspicious regions, supporting overworked clinicians by flagging cases that need immediate review
| Traditional Review | AI-Assisted Review |
|---|---|
| 30-60 min/case | 5-15 min/case |
| Human fatigue risk | Consistent accuracy |
| Variable outcomes | Reliable scoring |
AI-powered pattern recognition is speeding up the time from scan to answer, reducing delays when it matters most.
Reducing Human Error and Bias in Clinical Assessments
Human error happens—fatigue, busy schedules, or bias can all affect how cancer is spotted and staged. AI helps level the playing field because computers:
- Use the same method, every time, for every patient
- Blindly process images and records without being swayed by doctors’ assumptions or incomplete histories
- Find subtle signs across multiple data sources (like images, blood work, and records)
The result? Fewer missed cases and more consistent diagnoses, especially in busy or resource-limited settings.
Rapid Assessment of Large-Scale Patient Data
AI doesn’t just look at a single scan—it actively sifts through huge amounts of patient data, often in real time. In the past, going through imaging, lab tests, and past notes for one patient could take hours. Now, AI is capable of cross-checking:
- Imaging studies with genetic results
- Pathology reports with the latest clinical trials
- Historical cases for comparison
This lets clinicians focus on the big picture and catch things that aren’t obvious.
- Speed: Results delivered in minutes, not days
- Capacity: Hundreds of patient cases reviewed at once
- Insights: Finding correlations that humans would never spot
With AI on their side, care teams can make decisions faster and with greater confidence—giving patients a real shot at earlier treatment and better outcomes.
Personalizing Cancer Treatment Pathways Using AI in Cancer Diagnostics

AI is really changing how cancer treatment is tailored to each person. Unlike before, when treatment options followed a standard process, today, artificial intelligence helps doctors consider everything unique about an individual—genetic makeup, lab results, tumor features, lifestyle, and more. In 2025, AI isn’t just a tech add-on but a real part of patient care—giving doctors details and predictions they never had before.
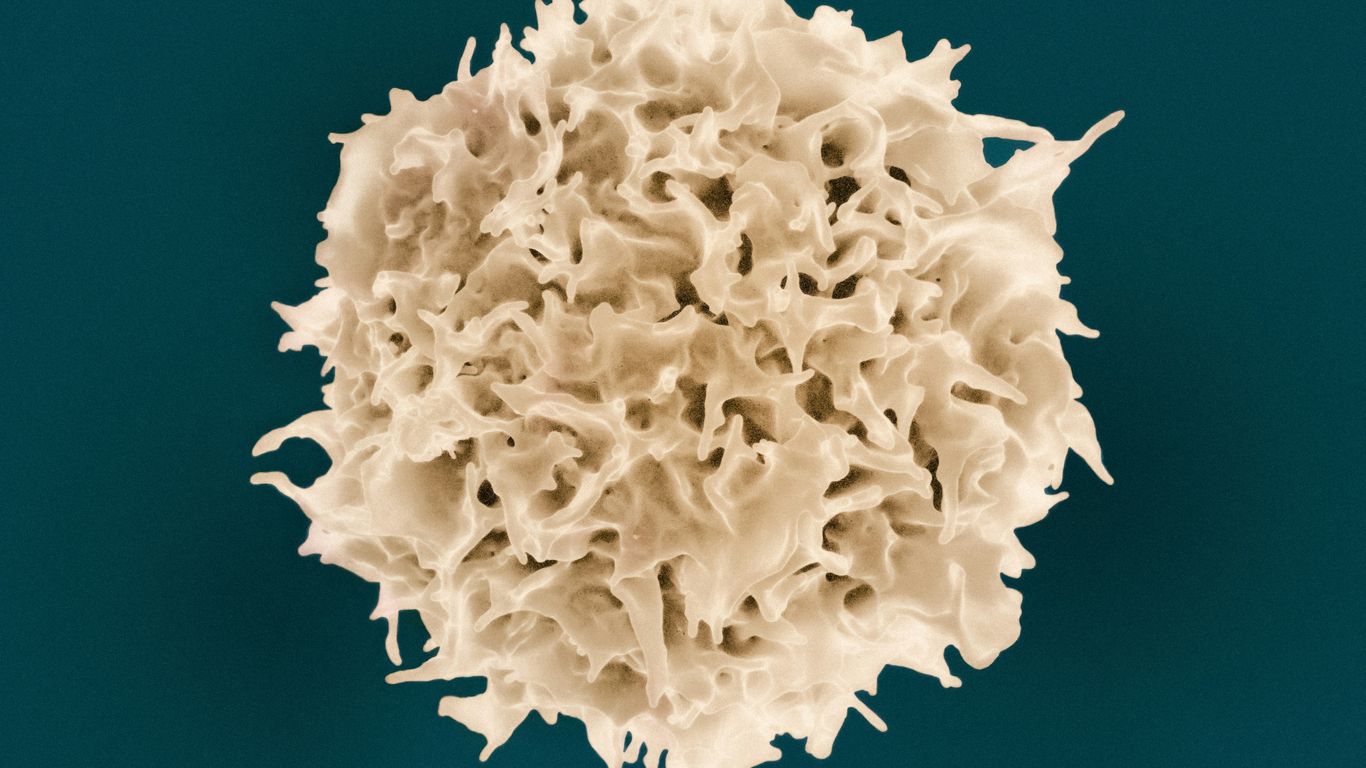
Genomic and Biomarker Analysis for Tailored Therapies
AI tools can now make sense of massive numbers of genetic and biomarker results. Algorithms quickly sift through gene sequences and protein markers, comparing them with global databases to spot mutations or traits that might influence which drugs will—or won’t—work. This approach can spare patients from side effects of treatments unlikely to help them and speed up finding better options.
Key points:
- Matches patients with drugs designed for their tumor type.
- Flags unusual mutations that might qualify someone for a clinical trial.
- Analyzes how likely a person is to respond to common treatments like immunotherapy or targeted agents.
Real-Time Decision Support for Clinicians
Imagine being in a doctor’s office, and they have a dashboard that pulls together your history, lab values, scans, and even data from your wearables. This is no longer some future fantasy. Decision support tools now give doctors up-to-the-minute answers, often comparing your case with thousands of similar cases. The AI can nudge the care team to order a test, adjust meds, or try a new approach.
"Treatment choices are now less about guesswork and more about what the data suggests will work best for you, right now."
Digital Twins and Simulation of Treatment Responses
The concept of a digital twin is honestly incredible. It’s like having a computerized version of a patient—a model created from all their data: genetics, imaging, history, and more. AI simulations can test out different treatments in the digital world to see how the real person might react. For doctors and patients, this means choosing paths with more confidence and, possibly, fewer surprises.
Table: How AI Personalizes Cancer Care
| AI Technique | What It Does | Result for Patient |
|---|---|---|
| Genomic Analysis | Finds mutations and drug sensitivities | More precise drugs |
| Decision Support Platforms | Combines data for real-time recommendations | Faster, data-driven choices |
| Digital Twin Simulations | Models potential outcomes of different treatments | Better planning, fewer side effects |
- AI is not just about speed—it’s about smarter choices.
- New treatments and trial opportunities can reach the right people faster.
- AI is helping avoid the trap of “one size fits all” medicine in cancer.
AI tools are making cancer care more personal than ever, blending treatment ideas with what works for each unique patient—sometimes before symptoms or side effects even start.
Expanding Access and Equity in Cancer Care with AI in Cancer Diagnostics
Artificial intelligence isn’t just about high-tech hospitals or luxury clinics—it’s changing how and where people get cancer care. In 2025, AI has started breaking down stubborn barriers, giving more folks a shot at early detection and fair treatment no matter where they live or what resources they have.
AI-Powered Tools for Underserved Populations
AI tools have been a real boost in places that used to get left behind. Now, local clinics in small towns and rural regions can use AI-enabled devices to screen for cancer, even without a specialist on site. Here’s how these tools are making a difference:
- AI software helps non-specialist staff spot suspicious lesions or flag urgent cases so patients aren’t stuck waiting.
- Automated analysis means fewer missed diagnoses and a lower chance of people slipping through the cracks.
- Community health workers can use AI-powered platforms to connect with remote experts for second opinions.
This is closing some big gaps in cancer screening and treatment.
Mobile Diagnostics and Cloud-Based Solutions
It’s not always easy to travel for tests, especially if you live miles from a hospital. Mobile diagnostics, powered by AI, are rolling out everywhere:
- Portable devices, like AI-driven smartphone microscopes, can check for cancers like cervical or skin right on the spot.
- Cloud software uploads scans instantly for analysis, bringing expert-level insights to any connected clinic or health post.
- People can get biomarker results or symptom checks through simple mobile apps or wearable sensors, no supercomputer needed.
Here’s a simple table showing the difference AI mobile diagnostics are making:
| Feature | Traditional Care | With AI Diagnostics |
|---|---|---|
| Location | Hospital-based | Any connected location |
| Expert Required | Always needed | Sometimes optional |
| Wait Time | Days to weeks | Minutes to hours |
| Access in Remote | Rarely available | Frequently available |
Standardizing Care Across Diverse Clinical Settings
AI doesn’t just improve care in one location; it helps everyone get the same quality of service no matter the setting. Standardization is key:
- Automated algorithms follow set guidelines, so test results and follow-up steps don’t depend on who’s on duty that day.
- Errors due to tiredness or lack of experience are less common since decision support systems offer reliable, second-by-second advice.
- Data from multiple clinics feed into shared databases, creating a bigger picture of what’s working and what isn’t.
By making trusted diagnostics widely available and lessening local differences, AI is leveling the playing field in cancer care. Now, patients don’t have to rely on luck or location to get a fair chance.
Ethical, Privacy, and Regulatory Considerations for AI in Cancer Diagnostics
Ensuring Data Security and Patient Consent
AI systems in cancer diagnostics process tons of sensitive personal health info. Protecting patient data and getting clear consent is more important than ever. Here’s what health centers and tech companies are dealing with right now:
- Securing health records with advanced encryption methods
- Using privacy-preserving techniques, like training AI models without moving raw data between hospitals (sometimes called “federated learning”)
- Clearly communicating how data will be used, stored, and potentially shared with patients
| Security Method | Practical Example | Main Benefit |
|---|---|---|
| Data Encryption | Securing medical images in transit | Prevents data breaches |
| Anonymization | Removing names from datasets | Reduces identification risk |
| Federated Learning | Local training at hospitals | No need to move raw data |
Even with extra legal requirements, the big test is really building patient trust. People want to be sure that their medical information is safe, and that they’re truly agreeing to how it’s being used.
Addressing Bias and Fairness in AI Algorithms
Bias in cancer diagnostics AI isn’t just about bad code—it usually comes from the data these algorithms are trained on. If software learns mostly from a single group, it might make mistakes or be less accurate for others. Tackling this requires some real changes:
- Collecting diverse and well-annotated datasets from different groups and clinical settings
- Routinely auditing algorithms for unfair outcomes and correcting them
- Being transparent about a model’s limitations and who it works for
Some important steps tech teams are following:
- Partner with clinics from varied regions and backgrounds
- Periodically check AI predictions for patterns of bias
- Publicly report findings, even if they’re uncomfortable
Navigating Regulatory Landscapes and Compliance
AI in medicine doesn’t fit into the traditional rulebooks quite so neatly. With algorithms that update themselves or work across global sites, regulators have their work cut out. Here’s what’s in the mix for 2025:
- Agencies now require clear evidence of real-world testing, not just computer simulations
- Some countries are writing new rules specifically for AI—expect more standards by region
- A single tool might need approval on both sides of an ocean, so companies are juggling multiple compliance efforts
A quick look at how regulations differ:
| Country/Region | Regulatory Focus | Recent Changes |
|---|---|---|
| United States | Clinical effectiveness; cybersecurity | FDA released new AI guidelines in 2023 |
| European Union | Transparency and explainability | AI Act impacts all diagnostic software |
| Japan | Post-market surveillance, patient rights | Stricter reporting requirements |
The pressure is on both developers and hospitals to keep pace. Extra paperwork and checks slow things down, but missing a step could mean pulling a lifesaving tool from clinic shelves. Even as the rules get clearer, everyone’s still learning as they go.
Emerging Trends and Future Directions in AI in Cancer Diagnostics
Everything in cancer care just keeps shifting—if you blink, you’ll miss a new algorithm, tool, or crazy idea. Today, the cutting edge goes far beyond old-school image reading. It’s about fusing genetic info, real-time data from wearables, and all kinds of clinical records, building AI systems that can predict, simulate, and learn as more people go through treatment. Here’s how the next wave is looking:
Multi-Omics Integration and Predictive Modeling
- AI is starting to mix data from multiple sources—genomics, proteomics, and even patient lifestyle info—to get a more complete picture of an individual’s cancer risk and likely response to treatment.
- This is not just about visual scans, but teasing out small molecular patterns from blood, tissue, and imaging—sometimes even before symptoms show up.
- New predictive models use different layers of biomarker data, making it possible to estimate who will respond well to specific therapies.
| Omics Layer | Data Used | Impact on Diagnostics |
|---|---|---|
| Genomics | DNA sequencing | Mutation detection, risk scoring |
| Proteomics | Blood protein profiles | Early marker discovery |
| Metabolomics | Small molecule analysis in samples | Identifying progression signals |
Integrating so much patient data can feel messy, but it actually brings doctors closer to predicting cancer’s course for each individual—not just what usually happens.
Adaptive Clinical Trials and Drug Discovery
With new algorithms, clinical trials don’t have to be set in stone. AI means:
- Real-time updating of trial groups as patient responses and genomic data come in
- Adaptive matching—patients get shifted to promising drugs
- Faster identification of who’s benefiting, shrinking the time between discovery and actual approval
You might see a company running several micro-trials at once, each targeting a slightly different patient population, all monitored by AI dashboards.
Continuous Learning Platforms for Ongoing Improvement
The latest AI systems aren’t fixed once released—they improve as more data arrives. These platforms:
- Learn from each new scan, pathology report, or treatment outcome
- Spot shifts in cancer trends—like resistance patterns—sooner
- Regularly push updates to clinicians, not just annual guideline changes
What’s wild: clinical teams might wake up to new diagnostic rules based on yesterday’s global patient results. The system is never static.
The future of cancer diagnosis with AI means smarter, faster changes, but also more unpredictability. Doctors and labs need to stay nimble, but the hope is all of this means catching cancer sooner and treating it smarter for everyone.
Conclusion
So, looking at where we are in 2025, it’s clear that AI is changing the way we find and treat cancer. Things that used to take days or weeks—like sorting through scans or genetic data—now happen in minutes. That means doctors can spot cancer earlier and figure out the best treatment for each person, not just a one-size-fits-all plan. It’s not perfect yet, and there are still hurdles, like making sure everyone has access and keeping patient data safe. But the progress is real. AI is helping doctors catch cancer sooner, make fewer mistakes, and give people care that fits their unique needs. As more hospitals and clinics start using these tools, it feels like we’re finally getting closer to a future where cancer isn’t such a scary word. There’s still work to do, but the direction is promising—and honestly, it’s kind of exciting to see what comes next.