Key Themes From The AI In Healthcare Conference 2022
This year’s AI in Healthcare Conference really zeroed in on what matters most when bringing these powerful tools into our medical world. It wasn’t just about the tech itself, but how it fits into the bigger picture of patient care and the daily grind of healthcare professionals.
Centering The Patient In AI Development
It sounds obvious, right? But a big point made throughout the conference was that patients need to be more than just an afterthought in AI development. We’re talking about involving them from the very start, not just when a product is almost ready. Think co-design and constant consultation. The goal is to build AI tools that truly serve patient needs, not just add another layer of complexity.
Elevating Mundane Tasks Through AI
We heard a lot about how AI can take over those repetitive, time-consuming tasks that bog down doctors and nurses. Automating things like scheduling, paperwork, or initial data entry might not sound glamorous, but it’s a huge deal.
Here’s a breakdown of what this means:
- Reduced Burnout: Freeing up clinicians from administrative burdens.
- More Patient Time: Allowing healthcare workers to focus on direct patient interaction and care.
- Increased Efficiency: Streamlining operations for smoother healthcare delivery.
Prioritizing Transparency And Patient Safety
This was a recurring topic. When we talk about AI in healthcare, trust is everything. Presenters stressed the need for clear explanations about how AI tools work, how patient data is handled, and what safeguards are in place.
Key aspects discussed included:
- Model Explainability: Understanding the ‘why’ behind AI-driven decisions.
- Data Privacy: Robust measures to protect sensitive patient information.
- Safety Protocols: Rigorous testing and validation to prevent harm.
Bridging The Gap Between AI Potential And Healthcare Adoption
It’s pretty clear that artificial intelligence has the potential to really change healthcare. We hear comparisons to electricity or fire, things that fundamentally altered how we live. But honestly, getting these powerful tools into actual hospitals and clinics is proving to be a slower process than many expected. There’s this big gap between what AI could do and what’s actually being used day-to-day.
Addressing The Lag In AI Tool Implementation
So, why aren’t we seeing AI everywhere in healthcare yet? It’s not for lack of trying, but adoption has definitely lagged behind the hype. A big part of the problem is that healthcare is a complex system, and introducing new technology isn’t like flipping a switch. We need to think about how these tools fit into existing workflows, how they interact with different electronic health records, and, of course, how they’re paid for.
Here are a few reasons why implementation is slow:
- Integration Headaches: Getting new AI software to talk nicely with old hospital systems can be a real headache. It’s not always plug-and-play.
- Training and Buy-in: Doctors and nurses need to be trained on how to use these tools, and they need to see the benefit. If it just adds more work or feels unreliable, they won’t use it.
- Cost and ROI: Developing and implementing AI can be expensive. Showing a clear return on investment, whether that’s better patient outcomes or cost savings, is tough but necessary.
Navigating The Noise Of Emerging AI Technologies
Walk into any tech conference these days, and you’ll hear about a million new AI tools. It’s a lot. For healthcare professionals, trying to figure out which of these are actually useful and which are just buzzwords can be overwhelming. There’s so much information, and it’s hard to tell what’s real and what’s just hype.
It feels like we’re wading through a lot of noise to find the actual signal. We need better ways to sort through the options and identify the AI solutions that are truly going to make a difference in patient care and hospital operations.
The Need For Clearer Ethical Frameworks
Beyond just making the tech work, we also need to be really clear about the rules of the road. Ethical considerations are paramount when we’re talking about patient data and health decisions. Who is responsible if an AI makes a mistake? How do we make sure AI tools are fair and don’t worsen existing health disparities? These aren’t easy questions, and the answers aren’t always obvious. Having clear guidelines and frameworks in place will help build the trust needed for AI to really take hold in healthcare.
Fostering Trust And Literacy In Healthcare AI

Building confidence in AI tools within healthcare isn’t just about making them work; it’s about making sure everyone involved understands them and trusts the process. This means being upfront about how these tools are made and used.
Transparency Across The AI Lifecycle
When we talk about AI in healthcare, transparency is key. It’s not enough for a tool to just be effective. People need to know how it was built, what data it learned from, and how their own information is being handled. This openness helps build confidence and encourages responsible use. Think about it like this:
- How models are trained: Knowing the data sources and methods used to train an AI can reveal potential biases.
- Data privacy and protection: Clear explanations on how patient data is secured and used are vital.
- Decision-making processes: Understanding the logic behind an AI’s recommendations, even if simplified, helps clinicians and patients feel more in control.
Without this clarity, it’s hard for anyone to truly rely on AI systems.
Guiding Innovation With Core Principles
As new AI technologies emerge, it’s easy to get caught up in the excitement. However, the conference stressed the importance of sticking to fundamental principles. These aren’t just buzzwords; they are the guardrails for responsible AI development and deployment in healthcare.
- Patient Safety: This has to be the absolute top priority. Any AI tool must demonstrably do no harm.
- Equity: AI should work to reduce health disparities, not widen them. This means careful attention to how AI performs across different patient groups.
- Effectiveness: Tools need to be proven to work and provide real benefits to patient care or healthcare operations.
These core ideas should guide every decision, from initial concept to final implementation.
Tailored Education For AI Stakeholders
AI isn’t just for tech experts anymore. Doctors, nurses, administrators, and even patients need to have a basic grasp of what AI is and how it functions in their care. The conference highlighted that one-size-fits-all education just doesn’t cut it. We need different approaches for different groups:
- Clinicians: Need practical training on how to use AI tools in their daily workflow, understand their limitations, and interpret their outputs.
- Patients: Require clear, simple explanations about how AI might be used in their treatment, what data is involved, and their rights.
- Developers and Policymakers: Need a deeper understanding of the ethical and safety considerations specific to healthcare AI.
Getting this education right means AI can be adopted more smoothly and safely, benefiting everyone involved.
Collaboration And Future Directions For AI In Medicine
It’s clear that getting AI to really work in healthcare isn’t just about building fancy algorithms. We need to think about how everyone involved can work together and what we should aim for down the road.
Cross-Sectoral Collaboration For AI Development
Getting AI tools from the lab into actual hospitals and clinics requires a lot of different people to team up. Think researchers, doctors, nurses, tech companies, and even patients themselves. Everyone has a piece of the puzzle. For example, a study looking at AI adoption found that health systems are trying to figure out their priorities, successes, and the roadblocks they face. This kind of information is gold for developers.
- Researchers bring the new ideas and the science.
- Clinicians know what’s actually needed on the ground and what will work in real patient care.
- Tech companies have the skills to build and scale the tools.
- Patients are the ones who will use these tools, so their input is super important from the start.
Without this kind of teamwork, we risk building AI that doesn’t quite fit or that people don’t trust.
Measuring Outcomes And Demonstrating Value
So, we’ve got these new AI tools. Great. But how do we know if they’re actually making things better? That’s where measuring outcomes comes in. It’s not enough to just say an AI can do something; we need to show it. This means looking at things like:
- How much time do doctors and nurses save?
- Are patient wait times shorter?
- Is the quality of care improving?
- Are there fewer medical errors?
Demonstrating clear value is key to getting more AI tools adopted widely. It helps convince hospital administrators and policymakers that the investment is worth it. It’s about moving beyond the hype and showing real-world results.
The Evolving Landscape Of Healthcare AI
The world of AI is changing fast, and healthcare is no exception. We’re seeing new types of AI, like agentic AI, which can take more action on its own. This brings up new questions about how we manage and use these advanced systems responsibly. The conference highlighted that while AI’s power is growing, we need to be wise about how we use it. It’s a race between technology getting more capable and us figuring out the best ways to apply it safely and ethically. We’re still figuring out the best ways to make sure AI in healthcare is transparent, fair, and actually helps people.
Real-World Applications And Scalable AI Solutions

It’s easy to get caught up in the hype around AI, but what’s actually happening on the ground in healthcare? This year’s conference really zeroed in on the practical side of things, showing how AI is moving beyond theory and into actual patient care and hospital operations. We’re seeing AI tackle some of the biggest headaches in the system, making things run smoother and, hopefully, leading to better health outcomes for everyone.
AI-Driven Administrative Task Automation
Let’s be honest, a lot of time in healthcare gets eaten up by paperwork and administrative duties. AI is stepping in to help lighten that load. Think about scheduling appointments, managing patient records, or even processing insurance claims. These are tasks that, while necessary, don’t require a doctor’s specialized skills. AI tools can handle a lot of this much faster and with fewer errors. This frees up valuable time for doctors and nurses to focus on what they do best: caring for patients.
Here’s a look at some areas where AI is making a difference:
- Streamlining Patient Scheduling: AI can optimize appointment booking, reducing wait times and no-shows.
- Automating Medical Coding: AI algorithms can accurately assign medical codes to patient encounters, speeding up billing.
- Managing Electronic Health Records (EHRs): AI can help organize and extract key information from vast amounts of patient data.
- Improving Claims Processing: AI can detect fraud and errors, making the claims process more efficient.
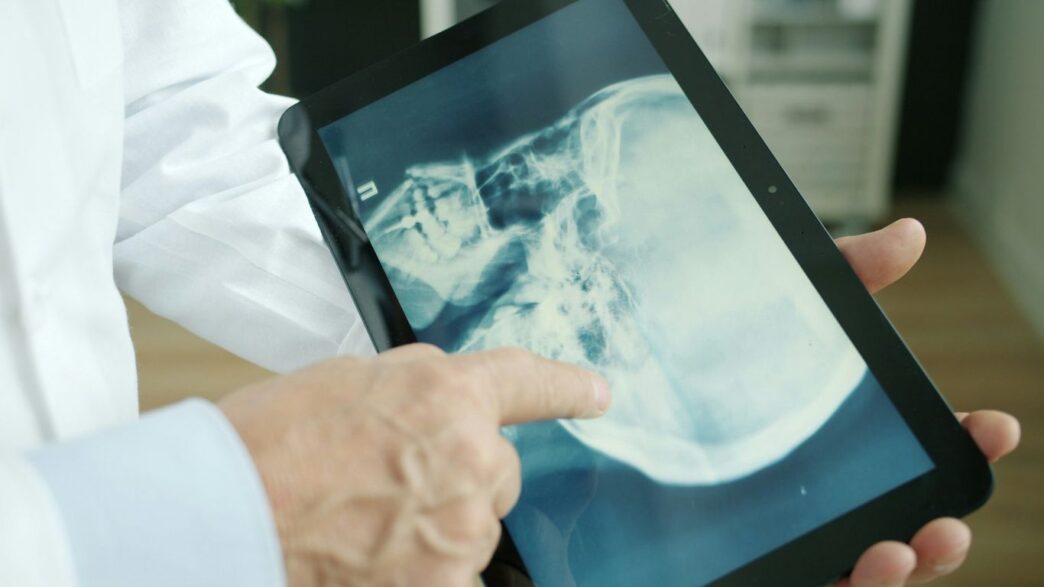
Patient Triage And Risk Stratification Tools
Getting the right care to the right patient at the right time is a constant challenge. AI is proving to be a game-changer here. Tools are being developed that can analyze patient symptoms and medical history to help decide the best course of action, whether that’s an immediate emergency room visit, a scheduled doctor’s appointment, or even remote monitoring.
This is particularly useful for:
- Early Detection of High-Risk Patients: AI can identify individuals who are more likely to develop certain conditions or experience complications.
- Prioritizing Care: In busy clinics or emergency rooms, AI can help sort patients based on the urgency of their needs.
- Personalized Treatment Pathways: By analyzing a patient’s unique data, AI can suggest tailored treatment plans.
The Rise Of Agentic AI In Clinical Settings
This is where things get really interesting. Agentic AI refers to AI systems that can take actions and make decisions autonomously. In healthcare, this could mean AI agents that monitor patients continuously, alert staff to critical changes, or even assist in complex procedures. While still in its early stages, the potential for agentic AI to support clinical decision-making and improve patient safety is huge. It’s about creating intelligent assistants that can work alongside healthcare professionals, providing real-time insights and support when and where it’s needed most.
Wrapping It Up
So, after all was said and done at the AI in Healthcare Conference 2022, it’s clear that while the tech is moving fast, actually getting it into hospitals and clinics is a whole other story. The big ideas were all about putting patients first, being upfront about how these tools work, and making sure they’re actually safe. Plus, a lot of talk focused on using AI to handle the boring, everyday tasks that eat up so much of doctors’ and nurses’ time. It’s not just about the flashy new stuff; it’s about making the whole system run smoother. There’s still a ways to go, especially when it comes to making sure everyone trusts these systems and understands them, but the conversations happening are definitely pointing in a more hopeful direction for how AI can help people get better care.