Dealing with pancreatic cancer can feel overwhelming, but there’s a lot happening in medicine that’s changing how we approach it. From finding it earlier to trying new treatments, doctors and scientists are working hard to make things better. This article talks about some of the latest ideas in pancreatic cancer diagnosis and treatment, hoping to bring some clarity and hope.
Key Takeaways
- New methods are improving how doctors find pancreatic cancer early on, which is a big deal.
- Treatments are becoming more specific, using things like genetic information to tailor care.
- Approaches like neoadjuvant therapy, given before surgery, are showing promise in shrinking tumors.
- Researchers are exploring how to get the body’s own immune system to fight pancreatic cancer.
- Clinical trials offer access to new treatments and are vital for advancing future care.
Advancing Pancreatic Cancer Diagnosis
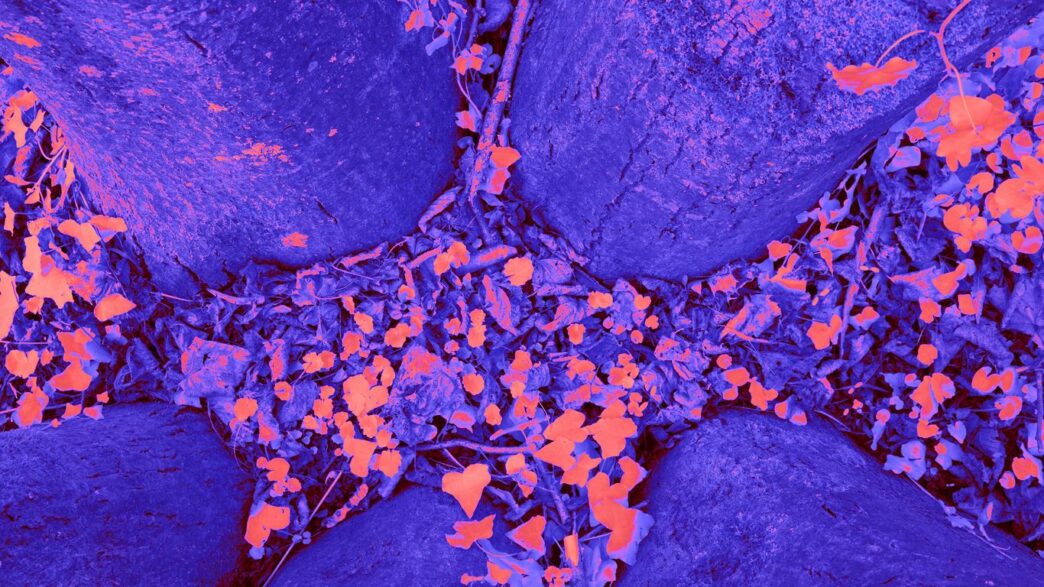
Understanding Pancreatic Cancer Cells
Pancreatic cancer starts when cells in the pancreas begin to grow out of control. The pancreas is a gland behind the stomach that helps with digestion and makes important hormones. Most pancreatic cancers, about 95%, are a type called pancreatic ductal adenocarcinoma. These often start with a change, or mutation, in a gene called KRAS. These cancer cells are tough. They can hide from treatments and grow fast, making them hard to catch early.
The Role of Genetic Testing
If you’re diagnosed with pancreatic cancer, talking about genetic testing with your doctor is a good idea. This test looks at your blood or saliva for changes in your DNA that you might have inherited. These inherited changes can raise your risk of developing certain cancers, including pancreatic cancer. The results can help your medical team figure out the best treatment plan for you. Plus, it can tell your family members if they might also be at a higher risk.
Here’s why genetic testing is becoming more important:
- Personalized Treatment: Some genetic mutations can be targeted with specific drugs.
- Family Risk Assessment: It helps identify relatives who may need increased screening.
- Understanding Cancer Origin: It can sometimes offer clues about how the cancer started.
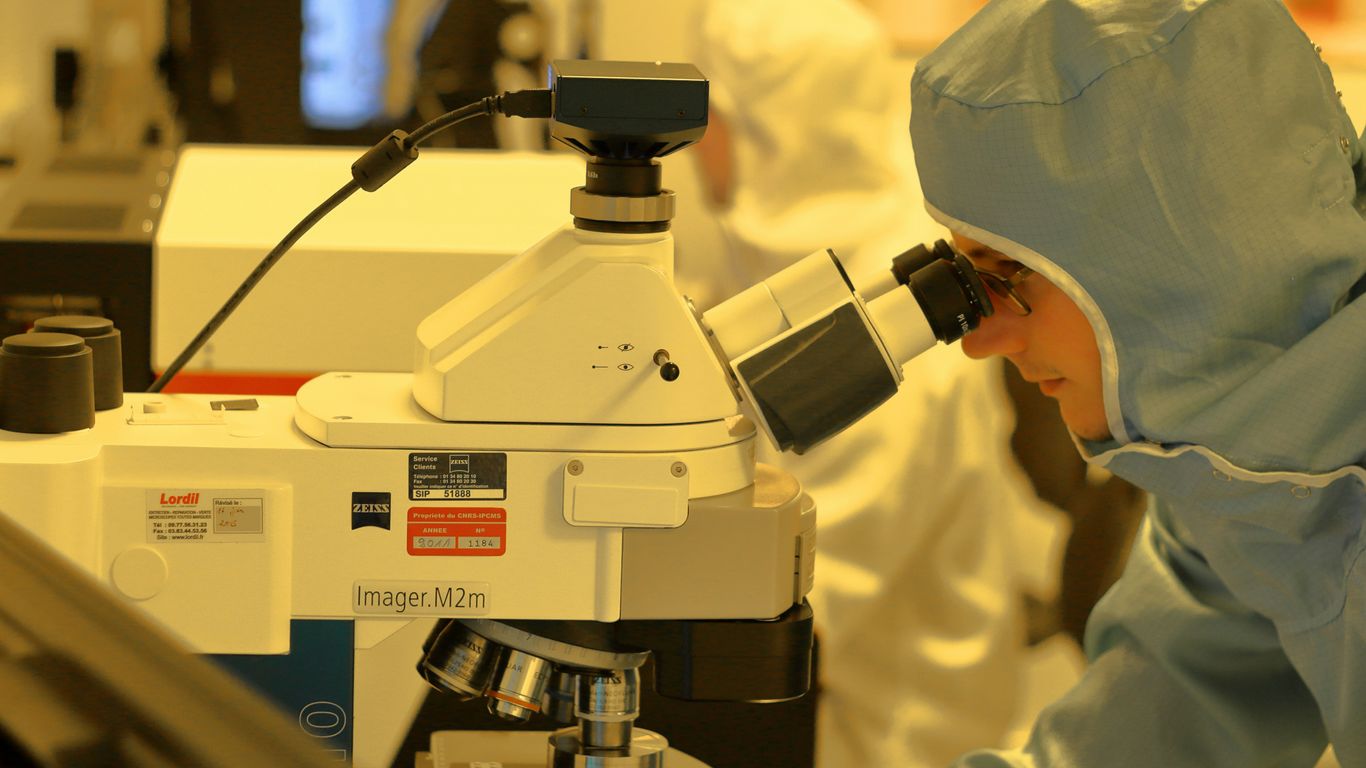
Diagnostic Imaging Techniques
To figure out if someone has pancreatic cancer and how far it has spread, doctors use different imaging tests. These tests create pictures of the inside of your body. Common ones include:
- CT Scans (Computed Tomography): These use X-rays to create detailed cross-sectional images.
- MRI Scans (Magnetic Resonance Imaging): These use magnets and radio waves to produce detailed images, especially good for soft tissues.
- Ultrasound: This uses sound waves to create images. Endoscopic Ultrasound (EUS) is a special type where a small ultrasound probe is attached to a thin tube that goes down your throat. It can get very close to the pancreas for clear pictures and is often used to take tissue samples.
- PET Scans (Positron Emission Tomography): These can help find cancer cells that may have spread to other parts of the body.
Sometimes, a biopsy is needed. This is where a small piece of tissue is taken, often during an EUS or with a needle, and sent to a lab to check for cancer cells and specific genetic changes. Blood tests, like one that looks for a marker called CA19-9, can also give clues, though they aren’t always reliable for everyone.
Evolving Treatment Strategies for Pancreatic Cancer
Neoadjuvant Therapy: A Pre-Surgical Approach
This is a big one. Instead of jumping straight to surgery, doctors are increasingly using treatments before the operation. This is called neoadjuvant therapy. It usually involves chemotherapy, sometimes with radiation, and the main idea is to shrink the tumor. Why is this good? Well, a smaller tumor is often easier to remove completely during surgery. This means a better chance for patients to get rid of all the cancer. It’s a shift from the old way of thinking, and it’s showing real promise in improving outcomes.
The Whipple Procedure and Surgical Options
When surgery is an option, the Whipple procedure (also known as a pancreaticoduodenectomy) is the most common operation for cancers in the head of the pancreas. It’s a complex surgery where a surgeon removes the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder, and the bottom part of the bile duct. Sometimes, a portion of the stomach is also removed. It’s a major operation, and recovery can be tough, but for many, it’s the best chance for a cure.
Other surgical approaches might be used depending on where the tumor is located and how far it has spread. Sometimes, a distal pancreatectomy (removing the tail of the pancreas) or a total pancreatectomy (removing the entire pancreas) might be necessary. The decision about which surgery is best is really tailored to each person’s specific situation.
Radiation and Chemotherapy Combinations
Chemotherapy and radiation are often used together, especially when surgery isn’t possible or after surgery to kill any remaining cancer cells. The combination can be quite potent. Doctors are getting smarter about how they use these treatments, often tailoring the dose and schedule based on the individual patient and the type of pancreatic cancer. Sometimes, they’re used in sequence with other treatments, like immunotherapy, to try and get the best possible result. It’s all about finding the right mix to fight the cancer effectively.
Precision Medicine in Pancreatic Cancer Care

Targeted Therapies for Specific Mutations
Pancreatic cancer is a tricky beast, and for a long time, treatment options felt pretty limited. But things are changing, and a big part of that is precision medicine. This means we’re getting smarter about how we treat the cancer by looking at its specific genetic makeup. For many pancreatic cancers, especially pancreatic ductal adenocarcinoma, a common culprit is a mutation in the KRAS gene. Targeted therapies are designed to go after these specific molecular flaws that drive the cancer’s growth. Think of it like having a special key for a very specific lock, rather than just a generic one. This approach aims to hit the cancer cells hard while being gentler on the rest of your body. Researchers are actively testing drugs that can block these mutated pathways, and early results are showing promise in slowing down or even shrinking tumors in some patients.
Personalized mRNA Vaccines
This is where things get really futuristic, but it’s happening now. You might have heard about mRNA technology with COVID-19 vaccines, but it’s also being explored for cancer. The idea with personalized mRNA vaccines for pancreatic cancer is to create a vaccine tailored specifically to your tumor. Scientists can analyze your tumor’s unique genetic signature and then create an mRNA vaccine that essentially teaches your own immune system to recognize and attack those specific cancer cells. It’s like giving your immune system a highly detailed
Harnessing the Immune System Against Pancreatic Cancer
The Potential of Immunotherapy
Immunotherapy has really changed how we treat a lot of cancers, basically teaching our own bodies to fight back. The idea is to get the immune system, especially those T-cells, to recognize and attack cancer cells. It’s a pretty neat concept, right? But pancreatic cancer has been a tough nut to crack for these treatments. It’s like the cancer cells have a secret handshake that makes them invisible to the immune system, or they actively shut down the immune response before it can even start. This makes it really hard for standard immunotherapies to get a foothold.
Overcoming Immune Evasion
So, why is pancreatic cancer so good at hiding? Well, it builds this sort of protective shield, a tumor microenvironment, that keeps immune cells out and even tricks them into thinking everything is fine. It’s a complex biological defense system that pancreatic cancer cells have developed. Researchers are looking into ways to break down this shield. This involves developing new drugs that can "release the brakes" on immune cells, allowing them to get in and do their job. It’s about making the cancer cells visible again and then giving the immune system the green light to attack.
Clinical Trials for Novel Immunotherapies
Because pancreatic cancer is so tricky, a lot of the exciting work is happening in clinical trials. These trials are testing out brand-new ideas. Some are looking at ways to engineer T-cells to be super-specific cancer hunters. Others are trying combinations of therapies to see if hitting the cancer from multiple angles works better. It’s a process of trial and error, but it’s where the real progress is being made.
Here’s a look at some of the approaches being explored:
- Checkpoint Inhibitors: These drugs block proteins that stop T-cells from attacking. Think of it like taking the parking brake off a car.
- CAR T-cell Therapy: This involves taking a patient’s own T-cells, modifying them in a lab to recognize cancer cells, and then putting them back into the patient.
- Oncolytic Viruses: These are viruses that are engineered to infect and kill cancer cells while also stimulating an immune response.
- Vaccines: Some experimental vaccines aim to train the immune system to recognize specific markers on pancreatic cancer cells.
The complexity of pancreatic cancer’s defense mechanisms means that a one-size-fits-all approach to immunotherapy just doesn’t cut it. Scientists are working hard to understand the unique ways each tumor hides and to develop treatments that can overcome these specific obstacles, offering more hope for patients.
The Critical Role of Clinical Trials
Expanding Treatment Options
Clinical trials are really the engine driving progress in how we treat pancreatic cancer. They’re where new ideas get tested, from brand new drugs to different ways of using treatments we already have. For patients, participating in a trial can mean getting access to therapies that aren’t available anywhere else yet. It’s a chance to be on the cutting edge of medical science. Think of it as being part of the solution, not just receiving care. Many trials are looking at combining different types of treatments, like using chemotherapy before surgery to shrink tumors, or exploring new ways to get the immune system to fight the cancer.
Accessing Innovative Therapies
When you’re dealing with pancreatic cancer, options can sometimes feel limited. Clinical trials open up a whole new set of possibilities. They are designed to test treatments that show promise in earlier research, aiming to improve outcomes for patients. This could involve new targeted drugs that attack specific weaknesses in cancer cells, or even personalized vaccines designed to train your own immune system to recognize and destroy the cancer. It’s a way to get treatments that are tailored to the latest scientific understanding.
Driving Future Research
Every person who joins a clinical trial contributes something significant, even if the treatment they receive doesn’t work for them personally. The data collected from these studies helps researchers understand what works, what doesn’t, and why. This information is absolutely vital for developing the next generation of treatments. Without people willing to participate, we wouldn’t have the breakthroughs we’ve seen so far, and we certainly wouldn’t be able to find cures in the future. It’s a collaborative effort that benefits everyone.
Participating in a clinical trial is a personal decision that requires careful consideration. It’s important to discuss the potential benefits and risks with your medical team and understand how the trial fits into your overall treatment plan. Your input and experience are invaluable to advancing cancer care for everyone.
Navigating Treatment Decisions
Deciding on the best path forward after a pancreatic cancer diagnosis can feel overwhelming. It’s a complex journey, and understanding the different aspects involved is key to making informed choices. This section aims to break down some of the important considerations.
Understanding Cancer Staging
Cancer staging is a way doctors describe how far the cancer has spread. It’s usually based on the size of the tumor, whether it has spread to nearby lymph nodes, and if it has spread to other parts of the body. The stage helps doctors figure out the best treatment options and gives an idea of the outlook.
- Stage 0: Very early cancer, often called carcinoma in situ.
- Stage I: Cancer is confined to the pancreas.
- Stage II: Cancer has spread to nearby lymph nodes or blood vessels.
- Stage III: Cancer has spread to major blood vessels or nerves around the pancreas.
- Stage IV: Cancer has spread to distant organs like the liver or lungs.
Knowing the stage is a critical first step in planning treatment.
Palliative Care and Symptom Management
Palliative care isn’t just for end-of-life situations; it’s about improving quality of life at any stage of a serious illness. For pancreatic cancer, this often means managing symptoms like pain, nausea, fatigue, and digestive issues. The goal is to make patients as comfortable as possible, allowing them to focus on treatment and daily life.
Effective symptom management can significantly impact a patient’s ability to tolerate treatment and maintain their well-being. It involves a team approach, often including doctors, nurses, dietitians, and social workers, all working together to address the patient’s physical and emotional needs.
Patient and Caregiver Support Resources
Facing pancreatic cancer is tough, and you don’t have to go through it alone. There are many places that can help both patients and their families.
- Information Handbooks: Resources like "Navigating Pancreatic Cancer: A Guide for Patients and Caregivers" offer detailed information on diagnosis, treatment options, and coping strategies. These guides can be downloaded or sometimes requested as a physical copy.
- Support Groups: Connecting with others who have similar experiences can be incredibly helpful. Organizations like the Pancreatic Cancer Action Network offer online and in-person support groups.
- Counseling Services: Sometimes, talking to a professional counselor, social worker, or spiritual advisor can provide much-needed emotional support.
- Clinical Trial Information: Websites and organizations dedicated to pancreatic cancer research often have sections to help patients find and understand clinical trials, which can offer access to the latest treatments.
Looking Ahead
It’s clear that the fight against pancreatic cancer is moving forward. New ways to find the disease earlier and treat it are popping up, thanks to dedicated researchers and doctors. Things like personalized medicine and new drug combinations are giving people more options than before. While there’s still a long road ahead, these advances offer real hope for better outcomes and a brighter future for those affected by this challenging illness. Staying informed and connected to support systems remains key as we continue to push for a cure.