Okay, so AI in medical stuff? It’s really taking off by 2025. Think smart tools helping doctors spot problems faster, keeping a closer eye on patients, and just generally making healthcare a bit smoother. It’s not just sci-fi anymore; these ai medical devices are actually showing up in hospitals and even on our wrists. But it’s not all simple – there are rules to follow, tricky tech bits, and we need to make sure everything is safe and fair for everyone. Let’s look at what’s happening.
Key Takeaways
- AI medical devices are becoming common, with thousands approved and a market growing into billions of dollars.
- Regulators worldwide are working on rules, but keeping up with fast-changing AI tech is a big challenge.
- AI is changing how we diagnose and monitor patients, showing up in everything from big imaging machines to small wearable gadgets.
- Concerns about data bias, patient privacy, and who’s responsible when AI makes a mistake are still major issues.
- The future holds even more advanced AI, like generative models, but balancing new tech with patient safety remains the main goal.
The Expanding Reach of AI Medical Devices
It feels like just yesterday AI in medicine was a futuristic idea, but now, by late 2025, it’s really becoming a standard part of how we do things in healthcare. Think about it: AI-powered tools are showing up everywhere, from the big imaging machines in hospitals to the little sensors on our wrists. The number of these devices getting the green light from regulators is climbing fast. The US FDA, for instance, has cleared thousands of AI/ML-enabled devices, and that number keeps growing by the month. It’s not just a few companies either; we’re seeing startups and huge medical tech giants alike jumping into this space.
Market Growth and Industry Trends
The market for AI in medical devices is booming. Analysts are putting the value in the billions, and they expect it to get much, much bigger in the next few years. This growth isn’t just about one type of device; it’s across the board. We’re seeing AI making its way into:
- Diagnostics and Imaging: AI algorithms are getting really good at spotting things in X-rays, CT scans, and MRIs, sometimes even better than the human eye. This means faster and more accurate diagnoses for things like cancer or eye diseases.
- Patient Monitoring: From hospital beds to home care, AI is helping keep a closer watch on patients. It can predict when someone might get worse, allowing doctors to step in sooner.
- Point-of-Care and Wearables: Devices you can use right at the doctor’s office or even wear yourself are getting smarter. Think smartwatches that can detect heart problems or continuous glucose monitors that predict sugar levels.
This rapid expansion means that AI is no longer a niche technology; it’s becoming a core component of modern medical equipment. Major players in the industry are integrating AI into their existing products, while new companies are bringing entirely novel AI-driven solutions to the table.
Key Stakeholder Perspectives
When you talk to different people involved, you get a range of opinions. Tech folks and some hospital leaders are pretty excited, pointing to all the data we have now and how AI has improved. Doctors, though, are often more cautious. They appreciate tools that can lighten their workload, but they’re also worried about getting too many false alarms or who’s responsible if something goes wrong. Patients generally want quicker results and better care, but they also want to know a human is still in charge and their personal information is safe. Meanwhile, insurance companies and hospital administrators are looking closely at the costs and what kind of return they can expect. Some big healthcare systems are even investing in their own AI research, hoping for long-term benefits.
The push for AI in medical devices is driven by a desire to improve accuracy, speed up diagnoses, and make healthcare more accessible. While the technology holds immense promise, its integration requires careful consideration of how it impacts the daily work of clinicians and the overall patient experience.
Geopolitical Influences on AI Adoption
It’s not just about the technology and the doctors; what’s happening in the world politically also plays a role. Governments around the globe are recognizing the importance of AI, especially in healthcare, and are putting policies in place to encourage its development. The US, for example, has been focused on leading the way and clearing roadblocks for innovation. Other countries, like those in the EU and China, are also pouring money into AI research, including in the medical field. For companies that make these devices, these global dynamics can affect things like where they get their parts, like the computer chips needed for AI, and what standards they have to follow. National interests are definitely tied to how health AI develops.
Navigating the Regulatory Landscape for AI Medical Devices
Keeping up with the rules for AI medical devices feels like trying to hit a moving target. It’s a complex area, and different countries are handling it in their own ways, though there’s a push to find some common ground. The main goal is always to make sure these devices are safe and actually work as intended, without stifling the innovation that could help so many people.
Global Harmonization Efforts
There’s a growing recognition that having completely different rulebooks everywhere makes things difficult for companies trying to get their devices approved globally. Organizations like the WHO and the International Medical Device Regulators Forum (IMDRF) are working on setting standards. They want to make sure that whether a device is approved in the US, Europe, or elsewhere, it meets certain benchmarks for safety, effectiveness, and how it’s managed throughout its life. This doesn’t mean a single, unified law, but more like a shared understanding of what’s important.
- Transparency: Knowing how the AI works and what data it was trained on.
- Validity: Proof that the device performs accurately and reliably.
- Lifecycle Management: Tracking the device from development through use and beyond.
- Risk Management: Identifying and mitigating potential harms.
The push for global standards aims to create a more predictable environment for AI medical device development and deployment. This is vital for both patient access and industry growth.
United States FDA Framework
The U.S. Food and Drug Administration (FDA) has been adapting its existing medical device regulations to fit AI. They’ve approved a significant number of AI/ML-enabled devices, with many going through the 510(k) pathway. A key development was their guidance on how to handle devices that learn and change over time, suggesting a "Predetermined Change Control Plan." This allows for updates without needing a full re-approval every single time, which is a big deal for AI that evolves. However, keeping tabs on how these devices perform after they’re out in the real world is still an area that needs more attention.
| Approval Pathway | Approximate Percentage (as of 2023) |
|---|---|
| 510(k) | ~97% |
| De Novo | <3% |
| PMA | Very small percentage |
Challenges in AI Medical Device Oversight
One of the biggest headaches is how to regulate devices that continuously learn and adapt. The traditional approval process wasn’t really built for software that can change its own behavior. Then there’s the issue of data bias – if the data used to train the AI isn’t representative of the whole population, the device might not work as well for certain groups. Making sure patient data is kept private and secure is also a constant concern. And when something goes wrong, figuring out who’s responsible – the developer, the doctor, the hospital? – can get really complicated.
- Adaptive AI: Regulating devices that change post-market.
- Data Bias: Addressing inequities in AI performance.
- Privacy & Security: Protecting sensitive patient information.
- Accountability: Determining liability for AI-related errors.
- Transparency: Understanding the AI’s decision-making process.
Clinical Integration and Adoption of AI Medical Devices
So, AI in medicine isn’t just a lab experiment anymore. It’s actually showing up in hospitals and clinics, and it’s changing how doctors and nurses do their jobs. The big idea is to make things faster, more accurate, and maybe even catch problems earlier than before. Think about it: AI can look at scans, monitor patients, and even help with paperwork, freeing up healthcare workers for more important stuff.
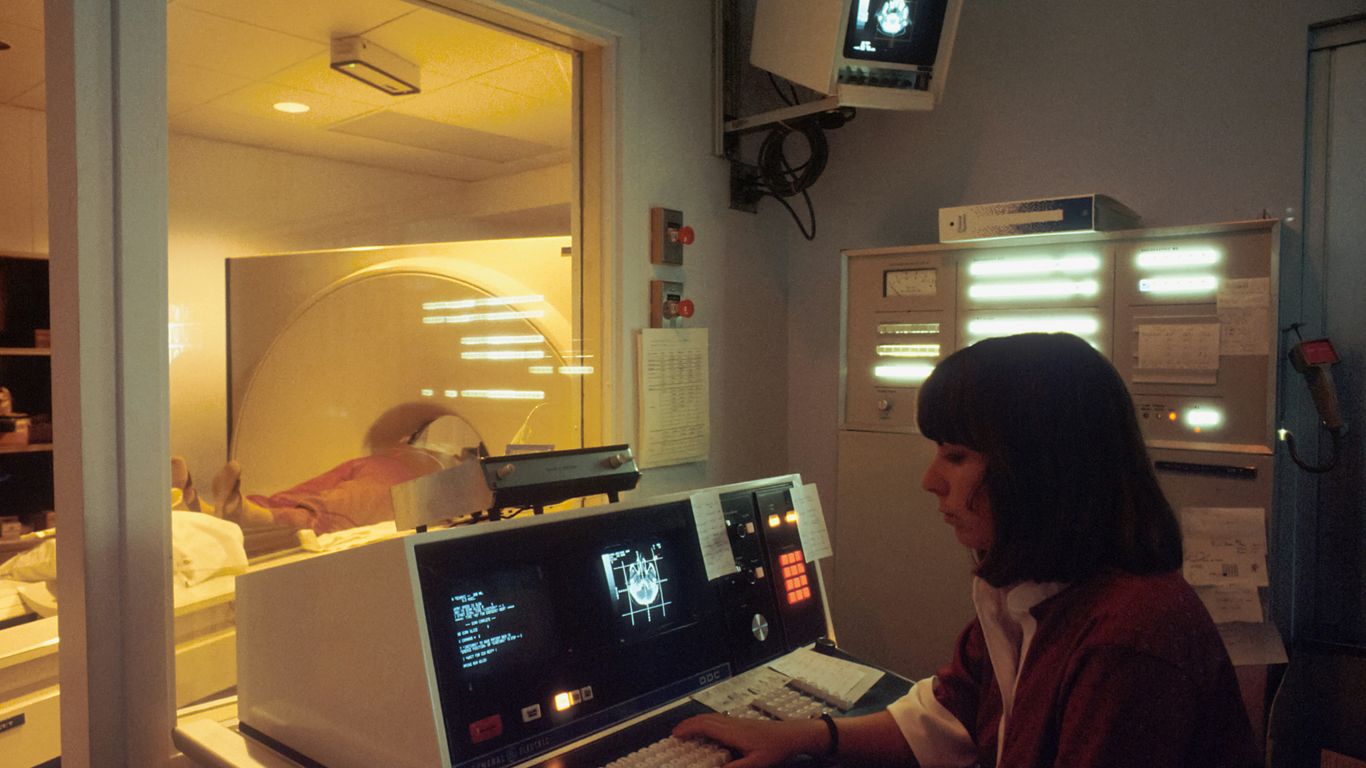
Transforming Diagnostics and Imaging
This is where AI is really making waves. Algorithms are getting pretty good at spotting things in X-rays, CT scans, and MRIs that a human eye might miss, especially when things are subtle or when a radiologist is swamped with cases. It’s not about replacing the expert, but giving them a super-powered assistant.
- Faster image analysis: AI can process scans in minutes, sometimes seconds, flagging urgent cases for immediate review.
- Improved detection rates: Studies show AI can help find early signs of diseases like cancer or diabetic retinopathy with greater accuracy.
- Reduced workload: By automating initial screenings, AI can help manage the sheer volume of imaging data healthcare systems produce.
Enhancing Patient Monitoring and Care
Beyond just looking at pictures, AI is also stepping in to keep a closer eye on patients, especially those with chronic conditions or those recovering from surgery. Wearable devices and sensors are collecting a ton of data, and AI is the key to making sense of it all.
The real challenge isn’t just building smart AI, but making sure it fits into the busy, often chaotic, world of a hospital or clinic. If a tool adds more steps or is hard to use, even the smartest AI won’t get picked up by busy doctors and nurses.
- Remote patient monitoring: AI can analyze data from home-based devices to alert clinicians to potential issues before they become serious.
- Predictive analytics: By looking at patient data, AI can help predict who might be at risk for certain complications, allowing for proactive care.
- Personalized treatment plans: AI can help tailor treatment strategies based on an individual’s specific data and response patterns.
AI in Point-of-Care and Wearable Devices
We’re also seeing AI pop up in smaller, more accessible devices. This means that advanced diagnostic capabilities are moving out of the big hospital labs and closer to the patient, sometimes even into their own hands.
| Device Type | AI Application |
|---|---|
| Wearable ECG | Arrhythmia detection, heart rate variability |
| Smart Stethoscopes | Heart murmur identification, lung sound analysis |
| Mobile Apps | Symptom checking, basic diagnostic assistance |
| Point-of-Care Tests | Automated analysis of blood or urine samples |
This shift is particularly exciting for areas with limited access to specialists. A doctor in a rural clinic, for instance, could use an AI-powered tool on a smartphone to get a preliminary analysis of a skin lesion or an eye scan, helping them decide if a patient needs to be referred to a specialist. It’s about democratizing access to advanced medical insights.
Addressing Risks and Ethical Considerations in AI Medical Devices
Okay, so we’ve talked a lot about how cool AI is for medicine, but we gotta slow down and think about the not-so-fun stuff. It’s not all sunshine and perfect diagnoses. There are some real worries we need to get a handle on before these things become as common as stethoscopes.
Data Bias and Algorithmic Transparency
One of the biggest headaches is bias. AI learns from data, right? Well, if the data it learns from isn’t diverse, the AI can end up being unfair. Imagine an AI trained mostly on data from one group of people. It might not work as well for someone from a different background. This could mean missed diagnoses or wrong treatments for certain patients. It’s like trying to teach a kid about the world using only books about one city – they’re going to have a pretty skewed idea of what’s out there.
- Need for Fairness Audits: Companies making AI tools should show that they’ve checked their systems for bias. This means looking closely at the data used and how the AI makes decisions.
- "Red Teaming" Exercises: Think of this like intentionally trying to trick the AI. You throw weird or tricky scenarios at it to see if it breaks or makes bad calls. It’s a way to find those hidden weak spots.
- Ongoing Monitoring: Just checking once isn’t enough. We need to keep an eye on how the AI performs in the real world to catch any new problems that pop up.
It’s really important that AI tools don’t just make things easier for doctors; they have to work well for everyone. If an AI tool is supposed to help decide who gets a certain treatment, it needs to be fair to all patients, no matter their race, gender, or where they come from. We can’t have systems that accidentally make health disparities worse.
Ensuring Patient Safety and Privacy
Then there’s the whole privacy thing. These AI systems often need access to a ton of sensitive patient information. We’re talking medical histories, scans, you name it. Keeping that data locked down is super important. Laws like HIPAA are there for a reason, and AI adds new layers of complexity. What happens if there’s a data breach? Or if the AI itself is tricked into giving up private info? Plus, do patients even know when an AI is involved in their care? Sometimes, it’s not clear, and that’s a problem.
Liability and Accountability for AI Errors
And what if the AI messes up? If a patient is harmed because an AI made a mistake, who’s on the hook? Is it the company that made the AI? The doctor who used it? The hospital that put it in place? The legal side of this is still pretty fuzzy. Right now, it often falls back on the doctor or the hospital. But as AI gets smarter and makes more decisions, we need clearer rules about who is responsible when things go wrong. It’s a complex web, and we’re still figuring out how to untangle it.
The Future Trajectory of AI Medical Devices
Emergence of Generative and Multimodal AI
We’re seeing AI move beyond just recognizing patterns. Think about generative AI, the kind that can create text or images. In medicine, this could mean AI helping doctors write patient reports faster, or even generating personalized treatment plans based on a patient’s unique data. Multimodal AI, which can process different types of information at once – like images, text, and patient history – is also a big deal. This means an AI could look at an X-ray, read the radiologist’s notes, and check the patient’s chart all at the same time to give a more complete picture. It’s like giving AI a much broader understanding of what’s going on.
Adapting Healthcare Systems for AI
Getting these advanced AI tools into hospitals and clinics isn’t just plug-and-play. Healthcare systems need to get ready. This involves a few key things:
- Training Staff: Doctors, nurses, and technicians need to learn how to use these new AI tools effectively and understand their limitations.
- IT Infrastructure: Hospitals need robust computer systems and networks that can handle the large amounts of data AI requires and ensure smooth integration with existing electronic health records.
- New Workflows: How AI fits into the daily routine of a doctor or nurse needs to be figured out. This might mean changing how patient information is reviewed or how diagnoses are made.
- Payment Models: Figuring out how to pay for AI-driven services is also a hurdle. Insurance companies and healthcare providers need clear guidelines.
Balancing Innovation with Patient Well-being
It’s a constant balancing act. On one hand, we want to push the boundaries of what AI can do in medicine, bringing new diagnostic and treatment possibilities to patients faster. On the other hand, patient safety and privacy have to be the top priority. We’ve seen thousands of AI medical devices get approved, but there’s still a lot to learn about their long-term impact and how to make sure they’re fair and unbiased for everyone.
The push for innovation in AI medical devices is strong, with companies and researchers eager to explore new capabilities. However, this drive must be carefully managed to avoid unintended consequences. The focus needs to remain on how these technologies can genuinely improve patient outcomes and healthcare access without introducing new risks or exacerbating existing inequalities. It’s about making sure the technology serves people, not the other way around.
The real challenge lies in creating an environment where AI can evolve rapidly while maintaining a strong ethical compass and rigorous safety standards. This means ongoing research, clear regulations, and open communication between developers, clinicians, patients, and regulators. By 2025, we’re seeing more collaboration, but the journey to fully integrate AI safely and effectively into everyday healthcare is still very much underway.
Wrapping It Up: What’s Next for AI in Medical Devices?
So, looking at where we are in late 2025, it’s clear that AI medical devices aren’t just a futuristic idea anymore; they’re a real part of how healthcare works now. We’ve seen tons of these tools get approved, and they’re showing up in hospitals and even in our homes. It’s exciting to see how they can help doctors spot problems earlier and make things more efficient. But, we’re still figuring out the best ways to make sure they’re safe, fair, and actually helpful for everyone. The next few years will be about learning from what works, fixing what doesn’t, and making sure these powerful tools are used responsibly. It’s a big job, but the potential to improve health for so many people makes it worth the effort.