It feels like every week there’s a new headline about a cyber attack, and the medical world is no different. Devices that help us stay healthy, or even save our lives, are increasingly connected to networks, which unfortunately makes them a target. This is where medtech cybersecurity comes in. It’s not just about protecting data anymore; it’s about making sure these devices work as they should and keep patients safe. Regulators are catching on, too, and are putting new rules in place. So, what does this all mean for companies making these devices and for us as patients?
Key Takeaways
- Cybersecurity needs to be a priority right from the start when designing medical devices, not something you add on later.
- The rules for medtech cybersecurity are changing all the time, and they’re different in places like the US and Europe, making it tricky to keep up.
- New threats are always popping up, like quantum computing, and companies need to think ahead to protect devices from future problems.
- It’s important to know who is involved in making your device, from the main manufacturer to smaller suppliers, and make sure they are also secure.
- Companies need to work with regulators and build security into their devices from the ground up to meet new requirements and keep patients safe.
The Evolving Landscape of MedTech Cybersecurity
It feels like just yesterday that cybersecurity was something companies tacked on at the end, if they thought about it at all. For medical devices, that approach just doesn’t cut it anymore. We’re seeing a big shift where security isn’t an add-on; it’s baked right into the recipe from the start. Think of it like building a house – you wouldn’t put the locks on after the walls are up and the paint is dry, right? It needs to be part of the blueprint.
Cybersecurity as a Core Design Consideration
This isn’t just a suggestion anymore; it’s becoming a requirement. Regulators are paying closer attention, and the threats out there are getting more sophisticated. Devices are more connected than ever, which means a vulnerability in one part can affect a whole system, potentially disrupting patient care. Manufacturers need to treat cybersecurity as a fundamental aspect of product development, not an optional extra.
Increasing Regulatory Demands Globally
Different countries and regions are putting out new rules and expectations. While some, like the FDA, are getting quite specific about what they want to see, others, like the EU with its MDR, are a bit more general. This means companies have to figure out how to meet various requirements, which can be a headache.
Here’s a quick look at what’s generally expected:
- Design Controls: Security measures need to be part of your design and development process.
- Risk Management: You have to identify potential security risks and figure out how to deal with them.
- Post-Market: Plans are needed to handle vulnerabilities that pop up after the device is already out there.
Emerging Threats and Future-Proofing Devices
We’re not just talking about today’s threats. There’s a lot of buzz about things like quantum computing, which could break current encryption methods down the road. Companies need to think ahead and build devices that can adapt to these future challenges. It’s about making sure your device is still secure years from now, not just when it ships.
The interconnected nature of modern medical devices means a security flaw can have widespread consequences, impacting not just the device itself but also patient data and the broader healthcare network. Proactive security measures are therefore paramount to maintaining patient safety and trust.
Navigating the Complex Regulatory Environment
The world of medical technology is always changing, and so are the rules that govern it. It feels like every time you get a handle on one thing, a new regulation pops up, especially when it comes to keeping devices safe and secure. This section looks at how companies are dealing with these shifting requirements, from the FDA’s specific rules to broader international standards. It’s a lot to keep track of, and honestly, it can feel overwhelming trying to stay on the right side of everything.
FDA’s Prescriptive Approach to Cybersecurity
The U.S. Food and Drug Administration (FDA) has been pretty clear about what it expects when it comes to medical device cybersecurity. They’ve put out guidance that’s pretty detailed, and it’s not just a suggestion; it’s something manufacturers really need to pay attention to. They want to see that cybersecurity is thought about from the very beginning of a device’s life, not just slapped on at the end. This means thinking about potential threats and how to build defenses right into the hardware and software. It’s a proactive stance, aiming to prevent problems before they can even happen.
- Early Integration: Cybersecurity needs to be a part of the design process from day one.
- Risk Management: Manufacturers must identify and address potential cybersecurity vulnerabilities.
- Post-Market Monitoring: Ongoing efforts are required to track and fix security issues that arise after a device is in use.
The FDA’s focus is on making sure that devices are secure throughout their entire lifespan, from the moment they’re conceived to when they’re eventually retired. This involves a lot of documentation and planning, which can add time and cost to development.
EU MDR and Generic Global Standards
Over in Europe, the Medical Device Regulation (MDR) is a big deal. It’s a comprehensive set of rules that covers a lot more than just safety; it includes cybersecurity too. While the FDA has its own specific guidance, the EU MDR often sets a higher bar and is seen as a benchmark that many other countries look to. It’s not just about meeting one country’s rules; it’s about understanding a framework that influences global standards. This means companies often have to design their devices to meet these stricter requirements if they want to sell them in multiple markets.
- Broad Scope: The MDR covers a wide range of safety and performance aspects, including cybersecurity.
- Stricter Requirements: It generally demands a higher level of evidence and documentation compared to previous regulations.
- Global Influence: Many countries are aligning their own regulations with the principles laid out in the MDR.
Harmonization Efforts by IMDRF
Trying to get all these different regulations to play nicely together is a huge challenge. That’s where groups like the International Medical Device Regulators Forum (IMDRF) come in. They work on trying to create common ground and harmonize standards across different countries. The idea is to make it easier for companies to get their devices approved in multiple places without having to reinvent the wheel each time. While they’ve made progress, especially with things like quality management systems, there’s still a long way to go. It’s a slow process, but any step towards making things more consistent is a good one for the industry.
- Common Frameworks: Developing shared approaches to device regulation.
- Reducing Duplication: Aiming to lessen the burden of multiple, conflicting regulatory reviews.
- Facilitating Global Access: Helping innovative devices reach patients worldwide more efficiently.
Key Regulatory Updates and Their Impact
Things are really shifting in the medical device world when it comes to rules and what companies need to do. It feels like every few months, there’s a new guideline or a change in how things are interpreted. It’s a lot to keep up with, honestly.
FDA’s Enhanced Premarket Cybersecurity Guidance
The FDA has been putting more focus on making sure medical devices are secure from the get-go. They’ve updated their guidance, and it’s not just a suggestion anymore. They want companies to really think about cybersecurity right when they’re designing a device, not as an afterthought. This means more documentation, more testing, and a clearer plan for how the device will stay safe from hackers and data breaches throughout its life. It’s a good thing for patient safety, but it definitely adds to the development time and cost.
- Proactive Risk Assessment: Companies now need to identify potential cybersecurity threats early in the design phase.
- Secure Development Practices: Implementing secure coding and testing throughout the development process is expected.
- Post-Market Monitoring Plans: A clear strategy for monitoring and addressing vulnerabilities after the device is released is required.
The emphasis is shifting from simply reacting to breaches to building devices that are inherently more resistant to attack.
EU’s Cyber Resilience Act and Certification Schemes
Over in Europe, they’re rolling out new rules too, like the Cyber Resilience Act. This act is pretty broad and applies to all sorts of digital products, including medical devices. It sets out requirements for security throughout the product’s life, from how it’s made to how it’s updated. They’re also looking at new certification schemes. This means devices might need specific cybersecurity certifications to be sold in the EU. It’s another layer of complexity, especially for companies selling globally, as they’ll need to meet different standards in different regions.
Post-Market Surveillance and Vulnerability Management
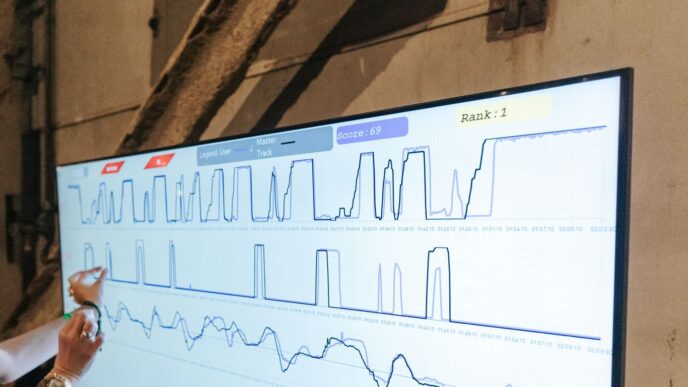
Once a device is out in the wild, the work isn’t over. Regulators are really pushing for better post-market surveillance. This means companies need to actively watch for any security issues that pop up after a device is in use. If a vulnerability is found, there needs to be a plan to fix it quickly, usually through software updates or patches. This ongoing management is becoming just as important as the initial design security. It requires dedicated resources and a commitment to transparency with both regulators and users about any discovered risks and how they’re being addressed.
Integrating Cybersecurity Throughout the Device Lifecycle
It’s easy to think of cybersecurity as something you bolt on at the end, like a final coat of paint. But with medical devices, that’s just not how it works anymore. Security needs to be part of the plan from the very first sketch to the moment the device is retired. This means thinking about potential weak spots and how to protect patient data and device function at every single step.
From Design to Decommissioning
Cybersecurity isn’t just a pre-market hurdle; it’s a continuous commitment. Manufacturers need to build security into the core architecture of their devices right from the start. This involves:
- Threat Modeling: Identifying potential threats and vulnerabilities early in the design phase.
- Secure Coding Practices: Implementing coding standards that minimize security flaws.
- Access Controls: Designing robust mechanisms to ensure only authorized users and systems can access device functions and data.
- Data Encryption: Protecting sensitive patient information both in transit and at rest.
The idea is to make security a foundational element, not an add-on. This proactive approach significantly reduces the likelihood of costly breaches and regulatory penalties down the line.
Lifecycle Management and Patching Strategies
Devices don’t stay static once they’re out in the field. New threats emerge, and software can develop issues. That’s why having a solid plan for managing the device’s entire lifespan is so important. This includes:
- Vulnerability Monitoring: Actively looking for newly discovered security weaknesses.
- Patch Development and Deployment: Creating and distributing updates to fix identified vulnerabilities.
- End-of-Life Planning: Defining how devices will be securely decommissioned to prevent data exposure.
Manufacturers must have a clear strategy for how they will provide security updates and patches throughout the expected operational life of their devices. This often involves setting up secure channels for updates and ensuring that older devices can still receive necessary security fixes.
Transparency in Cybersecurity Controls and Risks
Regulators are increasingly pushing for more openness about a device’s security features and potential risks. This means manufacturers need to be upfront with users and healthcare providers.
- Clear Documentation: Providing easy-to-understand information about the device’s security controls.
- Risk Disclosure: Communicating potential cybersecurity risks associated with the device’s use.
- Security Labeling: Offering guidance on how users can best manage the device’s security.
This transparency helps users make informed decisions and implement appropriate safeguards, contributing to a safer overall healthcare environment.
Addressing Specific Cybersecurity Risks
When we talk about keeping medical devices safe from hackers, it’s not just about the usual stuff anymore. There are some pretty big, new challenges popping up that we really need to pay attention to. It’s like the game keeps changing, and we have to keep up.
The Threat of Quantum Computing
This one sounds like science fiction, but it’s becoming a real concern. Quantum computers, when they get powerful enough, could break a lot of the encryption methods we use today to protect sensitive patient data. Think about it: all those years of medical records, treatment plans, and personal health information could suddenly be exposed. It’s not that current encryption is bad, but it’s like using a lock that worked fine yesterday, but tomorrow a new, super-powered tool might just pop it open. We need to start thinking about how to build devices that can handle this future threat, even if it seems far off.
- Quantum computers could make current encryption useless.
- This means sensitive patient data could be at risk.
- **Manufacturers need to plan for
Strategies for MedTech Cybersecurity Compliance
So, how do you actually make sure your medical tech is secure enough to pass muster with all these new rules? It’s not just about slapping on some antivirus software and calling it a day. You really need a plan, and it has to be thought out from the get-go.
Risk-Based Approach to Security
Think of it like this: not all parts of your device are equally tempting to hackers. Some functions are super critical, like controlling a pacemaker, while others might be less so, like a simple temperature display. A risk-based approach means you focus your security efforts where they matter most. You figure out what could go wrong, how bad it would be, and then you put the strongest protections on those high-risk areas. This way, you’re not wasting time and money on things that are already pretty safe. It’s about being smart with your resources.
- Identify critical device functions: What absolutely must be protected for patient safety and data privacy?
- Assess potential threats: What kinds of attacks are most likely against these functions?
- Prioritize security controls: Implement the most robust measures for the highest risks.
- Document your rationale: Be ready to explain why you chose certain security measures over others.
You can’t protect everything with the same level of intensity. It’s about making informed decisions based on what’s truly at stake for patient safety and the device’s integrity.
Collaborative Engagement with Regulators
Don’t just guess what the regulators want. Talk to them! Seriously, reaching out to bodies like the FDA or the EU agencies early in your development process can save you a lot of headaches later. They can offer insights into their expectations and help you understand their specific requirements. It’s better to get clarification upfront than to have your product delayed or rejected because of a misunderstanding. Think of them as partners in making sure your device is safe and secure for patients.
Security-By-Design Principles
This is a big one. Cybersecurity shouldn’t be an add-on; it needs to be built into the device from the very first sketch. This means thinking about security at every single step: when you’re choosing components, writing code, designing the user interface, and even planning how the device will be retired. It’s about making security a fundamental part of the device’s DNA, not just a feature you bolt on later.
- Secure coding practices: Train your developers and use tools to catch vulnerabilities early.
- Least privilege principle: Give software and users only the access they absolutely need.
- Secure defaults: Make sure the device ships with the most secure settings enabled out of the box.
- Regular security testing: Build testing into your development cycle, not just at the end.
It might sound like a lot of work, but getting it right from the start makes everything smoother down the line. Plus, it builds trust with your users and the regulators.
The Future of MedTech Cybersecurity
Looking ahead, the world of medical device cybersecurity is going to keep changing, and we all need to keep up. It’s not just about fixing problems after they happen anymore; it’s about building things right from the start and always being ready for what’s next. Staying ahead of cyber threats is now a non-negotiable part of bringing medical devices to patients.
Continuous Regulatory Awareness
Regulations are always being updated, and it’s a lot to track. Different countries and regions have their own rules, and they’re not always the same. For example, the FDA has specific ideas about what they want to see in device security plans, while the EU’s rules might be a bit more general, pointing to industry standards. It means manufacturers have to be really sharp about what’s required in every market they plan to sell in. It’s like trying to follow a dozen different instruction manuals at once.
- Keep a close eye on new guidance from agencies like the FDA and the European Medicines Agency (EMA).
- Understand how international standards, like those from IMDRF, are trying to make things more consistent.
- Be ready to adapt your security plans as new laws and recommendations come out.
Investing in Future-Ready Systems
We’re seeing new kinds of threats pop up all the time. Think about quantum computing – it’s still a ways off for widespread use, but it has the potential to break a lot of the encryption we use today. So, companies need to start thinking about how their devices will handle that down the road. It’s not just about protecting against today’s hackers; it’s about building systems that can withstand future challenges, even ones we can’t fully predict yet. This means looking at things like more robust encryption methods and designing systems that can be updated easily.
Fostering a Culture of Security
Ultimately, making sure medical devices are secure isn’t just an IT department’s job or a compliance team’s problem. It needs to be something everyone in the company thinks about, from the engineers designing the devices to the people selling them. When security is part of the company’s DNA, it’s much easier to make good decisions about device design and to respond quickly when a problem does arise. It’s about making security a habit, not a chore.
The trend is clear: cybersecurity is moving from a technical hurdle to a fundamental aspect of medical device quality and patient safety. Companies that treat it as such will be better positioned to succeed in the long run.
Looking Ahead: Staying Secure in a Connected World
So, where does this leave us? It’s pretty clear that cybersecurity isn’t just a tech problem anymore, especially in the medical device world. Regulators are really cracking down, and for good reason – patient safety is on the line. Manufacturers need to stop thinking of security as an add-on and start building it in from the ground up. It’s a lot to keep track of with all the different rules out there, but getting it right means safer devices and more trust from everyone. The future is connected, and staying ahead of cyber threats is just part of the job now. It’s about making sure the tech that helps us stay healthy doesn’t end up causing harm.