Okay, so I went to this big medical tech conference recently, and wow, there’s a lot happening. It felt like everyone was talking about the same few things, you know? From AI getting smarter to robots doing surgery and how we’re all supposed to connect our health stuff better. It’s a lot to take in, but basically, things are changing fast. Let’s break down what the big ideas were.
Key Takeaways
- AI is changing how we diagnose and treat illnesses, but we still need to figure out the trust and safety stuff.
- Robots and new tech are making surgeries less invasive and more precise, which is pretty cool for recovery.
- Getting new medical gadgets approved and out to everyone is a big hurdle, and companies need a solid plan.
- Digital health and remote doctor visits are becoming normal, but making them work with old systems is tricky.
- Wearable gadgets are now helping us keep an eye on health at home and catch problems early.
The AI Revolution in MedTech Dive
Artificial intelligence isn’t just a buzzword in medical technology anymore; it’s really starting to make things happen. We’re seeing AI move beyond the hype and become a core part of how new medical devices create value. People in the industry are talking about how AI is already helping in diagnostics, patient monitoring, and even creating new treatments. It’s got a lot of potential to change how we do healthcare.
Transforming Diagnostics and Therapeutics
AI is showing some serious promise in making medical diagnoses more accurate and faster. Think about image analysis – AI can spot things in scans that might be hard for the human eye to catch. This means earlier detection of diseases, which is always a good thing. On the treatment side, AI can help personalize therapies based on a patient’s specific genetic makeup or how they’re responding to treatment. It’s like having a super-smart assistant that can process vast amounts of data to suggest the best course of action.
Addressing Trust and Safety Concerns
Of course, bringing AI into healthcare isn’t without its challenges. A big one is building trust. Doctors and patients need to feel confident that AI systems are reliable and safe. There are also concerns about how effective these tools really are in real-world situations, not just in controlled lab settings. Making sure AI doesn’t introduce new biases or errors into healthcare is also a major focus. We need to be sure these systems are fair and work for everyone.
The Mean Time to AI Conversation
It feels like everywhere you turn, people are talking about AI. We’ve even heard the term ‘Mean Time to AI Conversation’ (MTTAIC) used to describe how quickly AI comes up in discussions about new medical tech. This shows just how central AI has become. It’s not just about using AI for diagnostics; it’s also about how it can speed up medical research and even change how patients interact with their healthcare providers. But as AI becomes more common, we have to keep cybersecurity and patient data privacy at the top of our minds. These issues need attention right away.
The path forward for AI in medicine involves careful development and testing. We need to make sure that as we integrate these powerful tools, we’re also building robust systems for oversight and accountability. It’s about finding that balance between innovation and responsible implementation.
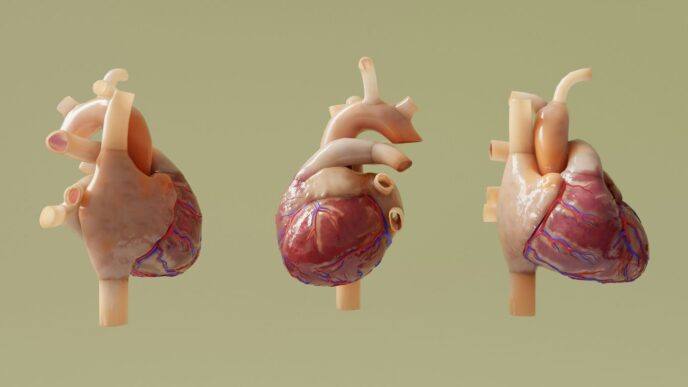
Advancements in Surgical and Neurotechnology
Minimally Invasive Techniques and Robotics
Surgery is getting less invasive, and robots are playing a big part. Think smaller cuts, quicker healing, and less pain for patients. We’re seeing new tools that can do things with incredible accuracy, like guiding tiny instruments through blood vessels or operating on delicate brain tissue. These aren’t just fancy gadgets; they’re changing how doctors approach complex procedures. The goal is to make surgeries safer and help people recover faster.
Here’s a look at some key areas:
- Robotic-Assisted Surgery: Robots are being used more and more to help surgeons perform procedures with greater control and precision. They can make very small, precise movements that a human hand might struggle with.
- Endoscopic Innovations: New endoscopes are smaller, more flexible, and equipped with better cameras, allowing doctors to see more and operate in tighter spaces without large incisions.
- Bioresorbable Materials: We’re starting to see implants and scaffolds made from materials that the body can absorb over time. This means fewer follow-up surgeries to remove devices.
The integration of robotics and advanced imaging is making complex surgeries more manageable, reducing the physical toll on patients and often shortening hospital stays significantly.
Neurotechnology for Enhanced Diagnostics
When it comes to the brain and nervous system, understanding what’s going on is half the battle. Neurotechnology is stepping up to the plate. Devices are being developed that can better detect early signs of neurological conditions, like Parkinson’s or epilepsy, sometimes even before symptoms become obvious. This early detection is a game-changer, allowing for earlier treatment and potentially slowing the progression of these diseases. It’s about getting a clearer picture of brain activity and function to help patients manage their conditions more effectively.
Precision Robotics for Soft Tissue Surgeries
Operating on soft tissues, like organs in the abdomen, has always been tricky. Now, precision robotics are making it much more manageable. These systems allow surgeons to manipulate instruments with extreme accuracy, even in confined areas. This means less damage to surrounding healthy tissue and a better outcome for the patient. Imagine a robot arm making tiny, steady movements to repair a delicate organ – that’s the kind of advancement we’re talking about. It’s about bringing a new level of control and finesse to surgeries that were once considered very high-risk.
Commercialization and Market Strategy
Bringing a new medical device from the lab to the people who need it is a whole process, and honestly, it’s way more complicated than just having a cool idea. You’ve got to figure out how to get it approved, how to make enough of them, and then how to actually get them into the hands of doctors and patients. It’s a big puzzle.
Navigating Regulatory Landscapes
This is probably the biggest hurdle for most MedTech companies. You can’t just slap a device on the market. There are rules, and they’re different everywhere you go. The FDA in the US has its own set of requirements, and then Europe has its CE marking, and other countries have their own systems too. It’s a lot to keep track of, and getting it wrong can set you back years or even kill your product.
- Understand the specific regulations for your device type. Is it a simple gadget or something that directly impacts patient health? That changes everything.
- Plan for global markets early. Don’t wait until you’re ready to launch to think about international rules. It’s much easier to build compliance in from the start.
- Engage with regulatory bodies proactively. Talking to them early, even before you have a finished product, can save a lot of headaches down the line. They can offer guidance that helps avoid costly mistakes.
Getting regulatory approval isn’t just a box to tick; it’s a fundamental part of building trust with both healthcare providers and patients. A well-thought-out regulatory strategy is a sign of a serious, responsible company.
Scaling Production for Global Reach
Okay, so you’ve got your approval. Now what? You need to actually make the thing, and not just a few. If your device is a hit, you’ll need to ramp up production significantly. This means finding reliable manufacturers, setting up quality control processes, and making sure your supply chain can handle the demand. It’s easy to underestimate how much capacity you’ll need, especially if you’re aiming for international sales.
| Stage | Key Considerations |
|---|---|
| Prototyping | Design for manufacturability, material sourcing |
| Pilot Production | Process validation, initial quality checks |
| Full-Scale Mfg. | Supply chain management, cost optimization, QC systems |
| Global Distribution | Logistics, warehousing, local compliance |
Achieving Long-Term Market Success
Getting the device out there is just the beginning. To really make it in the MedTech world, you need a solid plan for the long haul. This involves understanding how doctors and hospitals will actually use your device, how it fits into their workflow, and how they’ll pay for it. It’s not just about the technology; it’s about the entire ecosystem around it. Building relationships with key opinion leaders, gathering real-world evidence of your device’s effectiveness, and adapting to market changes are all part of the game. Success means making a lasting impact on patient care, not just a quick sale.
Digital Health and Telemedicine Integration
It feels like just yesterday we were talking about telemedicine as a new thing, and now it’s practically everywhere. But here’s the thing: just having virtual visits isn’t the whole story. We’re really talking about making these digital tools a normal part of how we get healthcare, not just a separate option. Think of it like this: your doctor’s office, your home, and your phone all working together. That’s the idea behind omnichannel healthcare – a connected experience.
The Rise of Omnichannel Healthcare
This is where things get interesting. Instead of just having a video call, we’re looking at how remote care fits into the bigger picture. It’s about making sure that whether you’re seeing a doctor in person, through a screen, or using an app, it all feels connected and makes sense. The goal is to create a patient journey that’s smooth, no matter how you interact with the healthcare system. This means your health records follow you, and your care team has a full view of your situation.
Reimbursement Framework Evolution
Let’s be honest, getting paid for these new ways of doing things has been a bit of a headache. The rules for how healthcare providers get reimbursed haven’t always kept up with the technology. We’re seeing a push to update these payment structures so that virtual visits and remote monitoring are recognized and paid for fairly. It’s a slow process, but it’s happening. Without fair reimbursement, it’s tough for these services to really grow and become a standard part of care.
Seamless System Integration Challenges
This is probably the biggest hurdle. Getting all these different digital health tools and existing hospital systems to talk to each other nicely is tough. Imagine trying to connect a brand-new smart device to a computer system that’s been around for ages – it’s not always straightforward. We need systems that can share information easily and securely. When systems don’t connect well, it can lead to mistakes, delays, and a lot of frustration for both patients and doctors.
The real work isn’t just creating cool new digital health tools; it’s making sure they actually work with the systems we already have and that people can get paid for using them. That’s where the actual progress happens.
Here are some of the key things we’re seeing:
- Better Patient Access: Digital health can reach people who might have trouble getting to a clinic.
- Data Sharing: Connecting different systems allows for a more complete view of a patient’s health.
- Efficiency Gains: Automating some processes can free up healthcare professionals’ time.
- Patient Engagement: Tools that let patients track their own health can lead to better outcomes.
Wearable Devices for Real-Time Monitoring
Bridging Home Care and Clinical Settings
It feels like just yesterday we were marveling at fitness trackers counting our steps. Now, wearable tech is doing so much more, really blurring the lines between what happens at home and what doctors see in the clinic. Think about it: devices that can keep an eye on your heart rhythm, blood sugar levels, or even sleep patterns, all from your wrist or chest. This constant stream of data is a game-changer for managing chronic conditions and spotting problems early. It means patients can be more involved in their own health, and doctors get a clearer picture of what’s going on between appointments.
Revolutionizing Patient Monitoring
This isn’t just about convenience; it’s about a whole new way to watch over people’s health. Instead of relying on snapshots taken during infrequent doctor visits, wearables provide a continuous flow of information. This allows for more personalized care plans and quicker adjustments when something isn’t quite right. The ability to track vital signs and other health metrics in real-time is transforming how we approach patient care, moving towards a more proactive and preventative model.
Here’s a look at what some wearables are tracking:
- Heart Rate Variability (HRV)
- Blood Oxygen Saturation (SpO2)
- Electrocardiogram (ECG) readings
- Activity levels and sleep quality
- Body temperature
Enabling Early Diagnosis and Insights
One of the most exciting parts of this technology is its potential for early detection. Subtle changes in your body’s signals, picked up by a wearable, could be the first sign of a developing health issue. This early warning system can lead to quicker diagnoses and interventions, potentially improving outcomes significantly. It’s like having a personal health detective working for you 24/7.
The data collected by these devices isn’t just raw numbers; it’s becoming a rich source of information that can help researchers understand diseases better and develop new treatments. The more data we gather, the smarter these systems become at identifying patterns and predicting health events.
Investment and Funding for Innovation
Getting new medical technology off the ground is tough. It takes a lot of brainpower, hard work, and, let’s be honest, cash. Investors are definitely watching the MedTech space, but they’re not just throwing money at any shiny new gadget. They want to see a real plan.
The Path to Reimbursement
This is a big one. If you can’t show how your innovation will get paid for by insurance or healthcare systems, investors get nervous. It’s not enough to have a great idea; you need a clear roadmap for how it fits into existing payment structures. Think about it: if doctors and hospitals can’t get reimbursed for using your device or software, they’re not going to adopt it, no matter how good it is. Demonstrating a viable reimbursement strategy is often the make-or-break factor for securing funding.
Investor Expectations for ROI
Investors are looking for a return on their money, and in MedTech, that means looking at both patient outcomes and financial gains. They want to see that your innovation can improve lives and be profitable. This often involves looking at:
- Market size: How many people can benefit from this?
- Scalability: Can this be produced and distributed widely?
- Competitive advantage: What makes this stand out from what’s already out there?
- Exit strategy: How will investors eventually get their money back (e.g., acquisition, IPO)?
Fueling MedTech Startups
So, how do startups actually get the capital they need? It’s a mix of different sources, and often requires a multi-stage approach. You might start with:
- Angel investors: Individuals who invest their own money, often early on.
- Venture capital (VC) firms: Professional firms that invest larger sums, usually after a company has shown some traction.
- Government grants and R&D tax credits: Non-dilutive funding that can help offset development costs.
- Strategic partnerships: Collaborating with larger companies that might invest or acquire.
The journey from a brilliant concept to a widely adopted medical device is long and complex. It requires not only groundbreaking technology but also a solid business plan, a deep understanding of the healthcare market, and the ability to convince both clinicians and payers of its value. Without this, even the most promising innovations can stall.
It’s a challenging landscape, for sure. But with the right approach and a clear vision, companies can find the support they need to bring their life-changing technologies to patients.
Navigating Regulatory and Compliance Hurdles

Getting a new medical device from the drawing board to someone’s hands is a journey filled with paperwork and rules. It’s not just about making something that works; it’s about making sure it’s safe and follows all the laws. This can feel like trying to solve a puzzle with missing pieces, especially when you’re dealing with new tech like AI or software that acts like a medical device.
Software as a Medical Device (SaMD)
Software that’s meant to be used for medical purposes, like diagnosing a condition or guiding treatment, has its own set of rules. These aren’t physical tools, but they have a big impact on patient care. The challenge is that software changes so fast. How do you regulate something that gets updated constantly? Agencies are working on this, but it means companies need to be extra careful about how they build, test, and update their SaMD. The key is to build safety and effectiveness into the software from the very beginning.
Global Regulatory Navigation
What’s approved in one country might not be in another. Each nation has its own health authority and its own set of requirements. For companies looking to sell their devices worldwide, this means a lot of different hoops to jump through. It’s a complex web of rules that can slow down how quickly a life-saving device reaches people who need it.
Here’s a look at some common areas of focus:
- Data Privacy: Protecting patient information is paramount.
- Cybersecurity: Connected devices need robust defenses against hacking.
- Clinical Evidence: Demonstrating the device’s safety and effectiveness through studies.
- Quality Management Systems: Implementing strong processes for manufacturing and development.
Early Engagement with Regulatory Bodies
Instead of waiting until your device is finished to talk to regulators, it’s often better to involve them early on. Think of it like getting advice from a coach before a big game. These conversations can help you understand what they’re looking for and avoid costly mistakes down the line. It can make the approval process smoother and faster.
Building a strong relationship with regulatory bodies isn’t about getting special treatment; it’s about clear communication and understanding expectations. This proactive approach can save significant time and resources, ultimately getting beneficial technologies to patients sooner.
This proactive approach helps clarify requirements and can lead to a more predictable path to market approval.
Looking Ahead
So, what’s the big picture here? It’s clear that medical technology is moving fast, and a lot of exciting stuff is happening. From smarter AI tools helping doctors and researchers to robots making surgery more precise, the goal is always to help people get better and stay healthier. We’re seeing more personalized solutions too, which is great for managing long-term health issues. Of course, it’s not all easy street. Getting these new ideas funded, figuring out all the rules, and making sure everything is safe and private are big jobs. But the drive to innovate is strong, and it seems like the industry is working hard to tackle these challenges. It’s going to be interesting to see how these advancements continue to change healthcare for all of us.