Dealing with medical coding can be a real headache, right? It’s a big part of how hospitals and clinics get paid, but it’s also super complicated and prone to mistakes. That’s where Nym AI comes in. They’ve developed this cool autonomous coding engine that uses smart technology to handle the coding process. Think of it as a super-fast, super-accurate assistant that takes the burden off the people working in healthcare, helping things run a lot smoother and hopefully making the whole money side of things less stressful.
Key Takeaways
- Nym AI uses a smart, multi-layered approach with AI to look at patient notes and figure out the right medical codes.
- This automation speeds up how quickly claims get processed, cutting down the time from start to finish.
- By reducing mistakes in coding, Nym AI helps lower the number of denied claims, which is a big win for hospital finances.
- The technology helps healthcare places use their staff better, letting coders focus on trickier jobs instead of routine tasks.
- Nym AI aims for over 95% accuracy and works to keep everything compliant with rules, making the whole billing process more reliable.
Understanding Nym AI’s Autonomous Coding Engine
The Multi-Layered AI Approach
Nym AI doesn’t just look at a medical chart and guess. It uses a few different AI technologies working together. Think of it like a team of specialists, each with a different skill. We’re talking about Natural Language Processing (NLP) to read and understand the doctor’s notes, machine learning to spot patterns, and deep learning to get even more precise. This layered approach means Nym AI can really dig into the clinical details and figure out the right codes. It’s a big step up from older systems that might have missed nuances.
Automated Code Application with Nym AI
Once Nym AI understands the patient’s record, it automatically applies the correct medical codes. This includes things like ICD-10-CM for diagnoses and CPT for procedures, plus any necessary modifiers. It does this based on the information it pulled from the chart. This whole process happens super fast, often in seconds, which is a huge change from how things used to be done. Instead of coders spending days on a stack of charts, Nym AI can process thousands in minutes. This speed and accuracy are what make it truly autonomous.
Nym AI’s Impact on Claims Processing Efficiency
When coding gets faster and more accurate, the whole claims process gets a boost. Think about it: if the codes are right from the start, fewer claims get kicked back. This means less back-and-forth with insurance companies and quicker payments. It also frees up the human coders to handle the really tricky cases that still need a human touch. This makes the whole operation run smoother and saves a lot of headaches.
Here’s a quick look at how Nym AI helps:
- Faster processing: Claims move through the system more quickly.
- Fewer errors: The automated system catches mistakes before they become problems.
- Better use of staff: Coders can focus on complex tasks instead of routine ones.
The shift to autonomous coding isn’t just about technology; it’s about rethinking how healthcare administration works. By automating the repetitive parts, we can focus human talent where it’s most needed, leading to better outcomes for everyone involved.
Revolutionizing Healthcare Revenue Cycles with Nym AI

The way healthcare organizations handle their finances, from the moment a patient is seen to when the bill is paid, is called the revenue cycle. It’s a complicated process, and frankly, it’s often a bottleneck. Nym AI is changing that by making this cycle much smoother and faster. This technology helps speed up the entire process, from start to finish.
Accelerating the End-to-End Timeline
Think about how long it takes for a claim to go from being generated to getting paid. It can feel like forever. Nym AI cuts down on that waiting time significantly. By automating the coding part, which is often a major delay, the rest of the process can move along much quicker. This means less time spent waiting for payments and more predictable cash flow for hospitals and clinics.
Reducing Errors and Denials Through Nym AI
One of the biggest headaches in the revenue cycle is claim denials. When a claim is denied, it has to be fixed and resubmitted, which costs time and money. Nym AI’s autonomous coding engine is designed to be super accurate. It reads through patient charts and assigns the correct codes the first time. This drastically cuts down on the mistakes that lead to denials.
Here’s a look at how Nym AI helps:
- Fewer Mistakes: The AI doesn’t get tired or overlook details like a human might. It consistently applies coding rules.
- Faster Processing: Claims with accurate codes get approved more quickly.
- Less Re-work: No need to spend hours fixing denied claims.
When claims are coded correctly from the start, the whole financial system for a healthcare provider runs better. It’s like having a well-oiled machine instead of one that’s constantly sputtering.
Optimizing Resource Allocation with Autonomous Coding
Manual medical coding takes up a lot of staff time. This time could be better spent on other important tasks, like patient care or complex billing issues. By letting Nym AI handle the bulk of the coding, healthcare facilities can reassign their skilled coders to focus on more challenging cases or other critical areas. This not only makes the coding process more efficient but also makes better use of the valuable human resources within the organization.
The Transformative Power of Nym AI in Medical Coding
Manual medical coding is a big part of why healthcare costs so much in the US. It’s a process that takes a lot of time and can lead to mistakes. Nym AI steps in here, changing how this whole thing works. It uses smart technology to look at patient charts and figure out the right codes, doing it way faster than people can.
Addressing Documentation-Coding Misalignment
Sometimes, what’s written in a patient’s chart doesn’t quite line up with the codes that need to be assigned. This can happen for a bunch of reasons – maybe the doctor’s notes are a bit unclear, or the coder misses a small detail. This mismatch is a headache because it can mess up billing and cause delays. Nym AI is built to understand the nuances of medical language. It can connect the dots between different parts of a patient’s record, making sure the codes accurately reflect the care provided. This ability to bridge the gap between documentation and coding is a game-changer.
Mitigating Downstream Financial Impacts
When coding goes wrong, it doesn’t just stop at the coding department. It causes a ripple effect that hits the hospital’s finances hard. Denied claims mean the hospital doesn’t get paid, and chasing those payments takes extra time and money. Nym AI helps prevent this by getting the codes right the first time. This means fewer claims get rejected, and the money comes in faster.
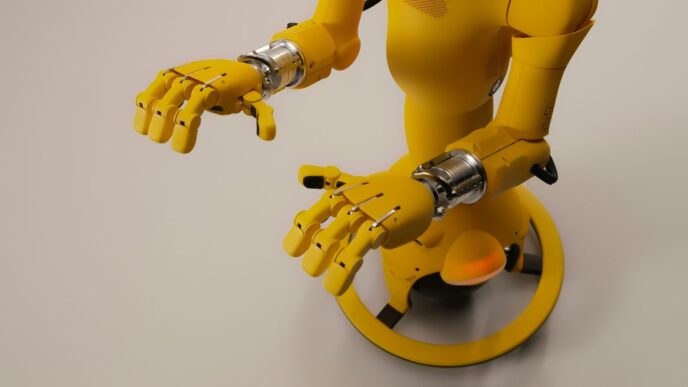
Here’s a look at how Nym AI impacts financial metrics:
| Metric | Improvement |
|---|---|
| Coding Accuracy | Over 95% |
| Claim Denial Rates | Reduced by 50% |
| Accounts Receivable Cycles | Shortened by 5 days |
| Revenue Capture | Increased by 5% |
Nym AI’s Precision and Speed in Chart Analysis
Think about how many charts a hospital deals with every day. A human coder has to read each one, understand it, and then find the right codes. It’s a slow process, and fatigue can set in. Nym AI, on the other hand, can process these charts in seconds. It doesn’t get tired, and its algorithms are designed to spot details that might be missed. This speed and accuracy mean that the coding process is no longer a bottleneck. It frees up staff to focus on more complex tasks or patient care, rather than getting bogged down in repetitive coding work.
The shift to autonomous coding isn’t just about saving money; it’s about making healthcare operations smoother and allowing medical professionals to concentrate on what they do best – caring for patients. This technology helps fix a system that’s often bogged down by administrative tasks.
Nym AI: Driving Financial Performance in Healthcare
Improving Financial Performance with Nym AI
Let’s talk about the money side of things. Healthcare providers are always looking for ways to keep their finances in good shape, and that’s where Nym AI really steps in. It’s not just about coding; it’s about making sure the whole system runs smoother so that money comes in when it should. Nym AI helps healthcare organizations get paid faster and more accurately. Think about it – less time spent chasing down payments or fixing mistakes means more resources available for patient care. It’s a pretty big deal when you consider how much administrative work goes into running a hospital or clinic.
Shortening Accounts Receivable Cycles
One of the biggest headaches in healthcare billing is waiting for payments. The longer a claim sits in accounts receivable, the more it can tie up cash flow. Nym AI tackles this head-on by speeding up the coding process. When codes are accurate from the start, claims are less likely to get held up or denied. This means less back-and-forth with insurance companies and a quicker path to getting paid.
Here’s a look at what Nym AI can do:
- Reduce the time it takes to get paid: Claims move through the system faster.
- Minimize claim rejections: Accurate coding means fewer reasons for denial.
- Improve cash flow: Money comes in more predictably.
The goal is to make the revenue cycle as efficient as possible, turning patient care into timely reimbursement without unnecessary delays or complications. This directly impacts the financial health of any healthcare provider.
Enhancing Revenue Capture Rates
Getting paid for the services you provide is obviously key. Sometimes, due to coding errors or missed documentation, healthcare providers don’t capture all the revenue they’re entitled to. Nym AI’s ability to analyze medical charts with precision helps to make sure every billable service is correctly coded. This means you’re not leaving money on the table.
- Accurate coding for all services: No more missed charges.
- Identification of all billable items: Captures the full scope of care provided.
- Reduced underpayments: Ensures fair reimbursement based on services rendered.
Implementation and Integration of Nym AI
Getting Nym AI up and running in your medical facility isn’t just about plugging in new software; it’s about thoughtfully weaving this autonomous coding engine into your existing operations. We’ve seen how a structured approach makes all the difference. The goal is to make the transition smooth, so your team can focus on what matters most – patient care.
Strategic Workflow Assessment for Nym AI
Before you even think about clicking ‘install’, it’s smart to take a good, hard look at how things work right now. Where are the slowdowns? How does the current coding process affect everything that comes after it, like billing and claims submission? Understanding these connections helps pinpoint exactly where Nym AI can make the biggest impact. It’s like planning a route before you start a long drive; you want to know the best way to get there.
Phased Implementation of Autonomous Coding
Jumping in headfirst with a full system-wide rollout might seem efficient, but often, a more gradual approach works better. Starting with a specific department or a particular type of medical service, especially those with high patient volume but less complex coding needs, lets you test the waters. You can measure the improvements in coding accuracy and speed, and see how it affects the whole claims process. This way, you learn and adjust as you go.
Here’s a possible way to think about phasing:
- Pilot Program: Select a single, high-volume department (e.g., outpatient visits).
- Performance Review: Analyze coding accuracy, processing time, and initial claim acceptance rates.
- Expansion: Based on pilot success, gradually roll out to other specialties like radiology or urgent care.
- Full Integration: Implement across all supported specialties.
Performance Monitoring and Staff Transition Planning
Once Nym AI is in place, the work isn’t over. You need to keep an eye on how it’s performing. This means tracking not just how accurate the codes are, but also how much faster claims are being processed and if denial rates are dropping. It’s also really important to think about your coding staff. This technology isn’t meant to replace people, but to change their roles. Planning for this transition involves figuring out how your experienced coders can move into more specialized tasks, like handling complex cases or auditing, freeing them from the more repetitive work.
Integrating Nym AI requires a clear plan that looks at both the technology and the people involved. By assessing current workflows, implementing in stages, and preparing your team for new responsibilities, you can make sure this powerful tool truly revolutionizes your medical coding process without causing unnecessary disruption.
Here’s a quick look at what you might expect:
| Metric | Potential Improvement |
|---|---|
| Coding Accuracy | Over 95% |
| Claims Denial Rate Reduction | Significant |
| Accounts Receivable Cycle | Shorter |
Nym AI’s Commitment to Accuracy and Compliance
Achieving Over 95% Coding Accuracy
Nym AI doesn’t just aim for good; it aims for great when it comes to medical coding accuracy. The system is built to get it right, consistently. We’re talking about an accuracy rate that often tops 95%, which is a big deal in an industry where small mistakes can snowball. This level of precision means fewer issues down the line with billing and insurance.
Ensuring Full Compliance with Nym AI
Staying compliant with all the ever-changing rules and regulations in healthcare is a constant challenge. Nym AI tackles this head-on. The engine is designed to keep up with updates from payers and regulatory bodies, automatically adjusting its coding practices. This means your organization stays on the right side of compliance without you having to constantly monitor every little change. It’s about building a system that inherently follows the rules.
Reducing Claim Denial Rates Significantly
High claim denial rates can really hurt a healthcare provider’s bottom line. Nym AI works to bring those numbers down, often by as much as 50%. How? By getting the codes right the first time. When codes are accurate and supported by clear documentation, claims are much more likely to be approved without a hitch. This leads to a smoother revenue cycle and less administrative back-and-forth.
Here’s a look at what Nym AI helps achieve:
- Improved Coding Accuracy: Consistently over 95% accuracy.
- Reduced Denials: Significant decrease in claim rejections.
- Streamlined Audits: Every code comes with a traceable audit trail.
The system generates a clear record for every code assigned. This includes the documentation that backs up the code and references to the guidelines used. It’s like having a detailed report card for each coding decision, making audits and compliance checks much simpler.
The Road Ahead
So, what does all this mean for the future of medical coding and healthcare in general? It looks like autonomous tech, like what Nym is doing, is really changing the game. We’re talking about faster claims, fewer mistakes, and letting our human experts focus on the really tricky stuff instead of getting bogged down in paperwork. It’s not just about saving money, though that’s a big part of it. It’s about making the whole system work better, so doctors and nurses can spend more time with patients and less time wrestling with administrative headaches. This shift to AI-powered coding is a big step forward, and it seems like it’s here to stay.