This article looks at how patient involvement has changed over time, especially with a focus on Context Media Health. We’ll explore how understanding what patients need, using new technology, and looking at real-world information helps make healthcare better for everyone. It’s all about making sure patients are a big part of their own health journey.
Key Takeaways
- Understanding what patients need and helping them get involved is super important for good healthcare.
- Using data from real patients helps us learn a lot about their health and how they manage it.
- Technology can help patients a lot, giving them tools and support for their health.
- Having patients work with researchers helps make studies better and more useful.
- Focusing on health results, not just products, helps make healthcare more valuable for people.
The Foundation of Patient-Centric Care
Understanding Patient Needs
To truly put patients first, we have to get a handle on what they actually need. It’s not just about treating symptoms; it’s about understanding the whole person. This means considering their background, their beliefs, and their daily lives. When we understand the patient’s perspective, we can tailor care that actually works for them.
- Active listening during appointments.
- Using surveys to gather feedback on experiences.
- Considering cultural and linguistic differences.
Bridging the Engagement Gap
There’s often a disconnect between what healthcare providers think patients need and what patients actually experience. This "engagement gap" can lead to frustration and poor outcomes. We need to find ways to close this gap by improving communication and building trust. It’s about making patients feel heard and valued. One way to do this is to focus on cultivating care through trust-based interactions.
Models of Engagement in Practice
Patient engagement isn’t just a buzzword; it’s something that can be put into practice in different ways. There are several models that healthcare organizations can use to improve patient involvement. These models often involve shared decision-making, where patients and providers work together to create a treatment plan. It’s about shifting from a paternalistic approach to one where patients are active participants in their own care. This can be achieved through virtual medical support.
Here’s a look at some common engagement models:
| Model | Description
Empowering the Modern Patient
Shifting Healthcare Dynamics
Healthcare isn’t what it used to be. Remember when doctors just told you what to do, and you did it? Those days are fading. Now, patients want to be involved, informed, and in control. This shift is driven by better access to information and a desire for personalized care. It’s not just about treating illness anymore; it’s about promoting wellness and helping people live healthier lives. This change affects everything, from how doctors interact with patients to how medical center management is handled.
Individual and Sociocultural Context
Healthcare isn’t one-size-fits-all. What works for one person might not work for another. We all have different backgrounds, beliefs, and lifestyles that affect our health decisions. Things like culture, income, and social support play a big role. For example, someone living in a rural area might have different healthcare needs and access compared to someone in a city. Understanding these individual and sociocultural factors is key to providing effective and equitable care. It’s about seeing the whole person, not just the disease.
Proactive Condition Management
Waiting until you’re sick to see a doctor? That’s so last century. Today, it’s all about being proactive. People are taking charge of their health by monitoring their conditions, making lifestyle changes, and seeking preventive care. This includes things like:
- Using wearable devices to track activity levels.
- Participating in online support groups.
- Adopting healthier diets.
This proactive approach not only improves health outcomes but also reduces the burden on the healthcare system. It’s about empowering individuals to take control and live their best lives. It’s about revolutionizing healthcare one step at a time.
Data-Driven Insights for Context Media Health
Leveraging Real-World Data
Okay, so, data. It’s everywhere, right? But in healthcare, it’s not just about numbers; it’s about people’s lives. Context Media Health really digs into real-world data to get a handle on what’s actually happening with patients. This means looking beyond the controlled environment of clinical trials and seeing how treatments and interventions play out in the messy, complicated world we all live in. Think about it: what good is a drug if people can’t stick to the dosage, or if it clashes with their lifestyle? Real-world data helps answer those questions. It’s about understanding the healthcare consumer journey and how people manage their health in their own environments.
Primary Research Methodologies
To get to the good stuff, you need to do some digging. Context Media Health uses a bunch of primary research methods to get direct insights from patients. This isn’t just about sending out surveys (though they do that too!). It’s about getting into the nitty-gritty with qualitative and quantitative research. Think focus groups, in-depth interviews, and even observing people in their natural habitats (ethnographic studies). It’s about understanding not just what people are doing, but why. Here’s a quick rundown of some methods:
- Surveys: Good for getting broad data on patient experiences.
- Interviews: Help uncover deeper motivations and feelings.
- Ethnographic Studies: Observing patients in their daily lives to understand behaviors.
Observational Healthcare Studies
Observational studies are a big deal. They let researchers watch what happens to patients without intervening directly. It’s like being a fly on the wall, but with data collection. This is super useful for understanding how diseases progress, how treatments work in the real world, and what factors influence patient outcomes. It’s not about testing a new drug; it’s about seeing how existing treatments are actually working. These studies can look at all sorts of things, like patient behavior, health outcomes, and even cultural differences that affect how people manage their health. It’s all about getting a complete picture of what’s going on.
Advancing Clinical Research Through Engagement
Patients as Research Partners
It’s time to stop thinking of clinical research as something done to patients and start seeing it as something done with them. The shift towards patient-centered research is gaining momentum, recognizing that patients bring unique insights and perspectives that can significantly improve study design, conduct, and outcomes. Think about it: who knows more about living with a condition than the people who actually have it? Their input can help researchers ask better questions, choose more relevant endpoints, and develop interventions that are truly meaningful.
Here’s how patients are stepping up as research partners:
- Advisory Roles: Patients are joining advisory boards, providing feedback on study protocols and materials. This ensures that research is understandable and addresses patient priorities.
- Steering Committees: Some patients are now full members of steering committees, actively participating in decision-making throughout the research process. This gives them real influence over the direction of the study.
- Co-Investigators: In some cases, patients are even serving as co-investigators, helping to design and conduct research projects. This is the ultimate level of partnership, where patients are fully integrated into the research team.
Integrating Biometric Monitoring
Biometric monitoring is becoming a big deal in clinical research, and it’s not just about fancy gadgets. It’s about getting a more complete picture of a patient’s health in real-time. Wearable sensors and other devices can track things like heart rate, activity levels, sleep patterns, and even glucose levels. This data can be incredibly valuable for understanding how treatments are working and identifying potential problems early on. The use of biometric data is growing rapidly.
But here’s the thing: it’s important to make sure that patients are comfortable with this technology and that their data is protected. Researchers need to be transparent about how the data will be used and give patients control over their information. If done right, biometric monitoring can lead to more personalized and effective treatments.
Non-Interventional Study Approaches
Not all clinical research involves giving patients a new drug or treatment. Non-interventional studies, also known as observational studies, are becoming increasingly popular. These studies involve collecting data on patients’ health without actively intervening in their care. This can be done through surveys, medical records, or even social media. The goal is to understand how diseases progress, identify risk factors, and evaluate the effectiveness of existing treatments in the real world. These studies are great for patient engagement because they don’t require patients to undergo any invasive procedures or take any new medications.
Here are some examples of non-interventional study approaches:
- Retrospective Chart Reviews: Researchers analyze existing medical records to identify patterns and trends.
- Prospective Observational Studies: Researchers follow a group of patients over time, collecting data on their health and lifestyle.
- Patient Registries: Researchers create databases of patients with specific conditions, collecting data on their demographics, medical history, and treatments.
These approaches can provide valuable insights into patient outcomes and help to improve healthcare delivery.
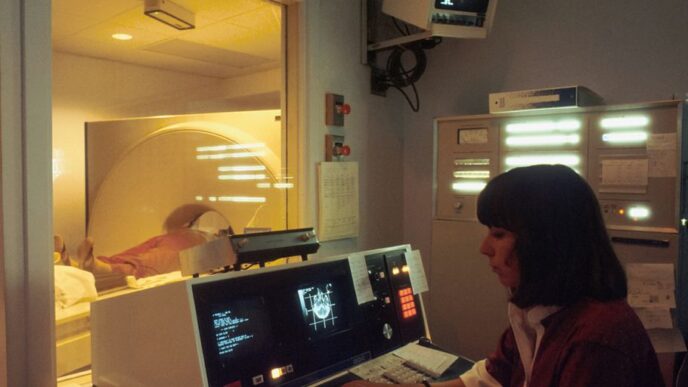
The Role of Technology in Patient Engagement

Technology is changing how healthcare works, and patient engagement is no exception. It’s not just about fancy gadgets; it’s about making healthcare more accessible, convenient, and effective for everyone. Think about it: from scheduling appointments to monitoring your health, tech is playing a bigger role than ever before.
Intelligent Technologies for Health
Intelligent technologies are revolutionizing healthcare by providing personalized and proactive solutions. We’re talking about things like AI-powered diagnostic tools, wearable sensors that track vital signs, and smart devices that help manage chronic conditions. These technologies can analyze huge amounts of data to identify patterns, predict potential health issues, and tailor treatments to individual needs. It’s like having a personal health assistant available 24/7. For example, AI-powered diagnostic tools can help doctors detect diseases earlier and more accurately, leading to better outcomes.
Digital Tools for Patient Support
Digital tools are making it easier for patients to stay informed and connected with their healthcare providers. Here are some examples:
- Mobile apps: These apps allow patients to schedule appointments, request prescription refills, access medical records, and communicate with their doctors through secure messaging. It’s all about convenience and accessibility.
- Telehealth platforms: Telehealth is booming, and for good reason. It allows patients to consult with doctors remotely, saving time and travel costs. It’s especially useful for people in rural areas or those with mobility issues.
- Online support communities: These communities provide a space for patients to connect with others who have similar conditions, share experiences, and offer support. It’s a great way to feel less alone and get advice from people who understand what you’re going through.
Transforming Clinical Trials
Technology is also transforming clinical trials, making them more efficient and patient-centered. Here’s how:
- Remote monitoring: Wearable sensors and mobile apps allow researchers to collect data from patients remotely, reducing the need for frequent in-person visits. This makes it easier for patients to participate in trials and improves data accuracy.
- Virtual trials: Some clinical trials are now conducted entirely online, using digital tools to recruit participants, collect data, and deliver interventions. This expands access to trials and reduces costs.
- Data analytics: Advanced analytics tools help researchers analyze trial data more quickly and identify trends that might otherwise be missed. This speeds up the drug development process and leads to better treatments. The use of remote monitoring in clinical trials is a game-changer, allowing for more continuous and real-world data collection.
Measuring Outcomes and Value in Healthcare
From Products to Outcomes
It used to be all about the latest drug or device. Now, the focus is shifting. Healthcare is increasingly about results, not just what’s being sold. This change is happening because of globalization, changing populations, new healthcare laws, better technology, and a real push for value. It’s not enough to have a great product; it needs to make a real difference in people’s lives. Understanding the drivers of health outcomes is key to optimizing patient research needs and commercial opportunities.
Assessing Patient Reported Outcomes
How do you know if something is working? Ask the patient! Patient-reported outcomes (PROs) are a big deal. They give us direct insight into how patients feel and function. It’s not just about what the doctor sees; it’s about the patient’s experience. This includes things like:
- Quality of life
- Pain levels
- Emotional well-being
- Ability to perform daily activities
Using PROs helps us get a more complete picture of a treatment’s effectiveness. It also makes patients more involved in their own care. It’s about AI-powered Revenue Cycle Management and understanding the healthcare consumer journey.
Value-Centric Healthcare Solutions
What does "value" even mean in healthcare? It’s about getting the best possible outcome for the lowest possible cost. This means:
- Focusing on prevention to avoid costly treatments later.
- Using resources wisely to eliminate waste.
- Making sure patients get the right care at the right time.
Value-centric solutions require a team effort. Doctors, patients, and insurance companies all need to work together. The goal is to create a system that’s both effective and affordable. It’s about primary research methodologies and ensuring every perspective can shape the understanding of what happened, and then guide the actions required for healing and learning.
Future Directions for Context Media Health
The Next Decade of Engagement
Looking ahead, Context Media Health is poised to keep pushing the boundaries of patient engagement. The next ten years will likely see a greater emphasis on personalized experiences, driven by advances in AI and machine learning. We’re talking about tailoring content and support to individual needs and preferences like never before. This means moving beyond generic health information to deliver resources that truly resonate with each patient’s unique circumstances. It’s not just about reaching more people, but about connecting with them in a more meaningful way.
Continuous Improvement Strategies
To stay ahead, Context Media Health needs to embrace a culture of continuous improvement. This involves:
- Regularly evaluating the effectiveness of engagement strategies using data-driven insights.
- Actively seeking feedback from patients and healthcare providers to identify areas for enhancement.
- Staying up-to-date with the latest research and best practices in patient engagement.
- Adapting to changes in the healthcare landscape, such as new technologies and evolving patient expectations.
It’s about constantly refining our approach to ensure we’re delivering the most impactful and relevant health information possible.
Sustaining Patient Partnerships
At the heart of Context Media Health’s mission is a commitment to building strong, lasting partnerships with patients. This means:
- Involving patients in the design and development of engagement programs.
- Creating opportunities for patients to share their stories and experiences.
- Providing ongoing support and resources to help patients manage their health.
- Advocating for policies and practices that promote patient-centered care.
Ultimately, it’s about recognizing that patients are not just recipients of care, but active participants in their own health journeys. By working together, we can create a healthcare system that is more responsive, more effective, and more human.
Conclusion
So, what does all this mean for patient engagement? It’s pretty clear that things are always changing. Context Media Health has been a big part of that change, helping to make sure people get the information they need. It’s not just about giving out facts; it’s about making sure those facts actually help people in their day-to-day lives. As we go forward, the goal is to keep making things better for patients. That means finding new ways to connect with them and give them what they need to be active in their own care. It’s a journey, and we’re still figuring things out, but the direction is good.
Frequently Asked Questions
What exactly is Context Media Health?
Context Media Health is a company that focuses on helping patients get more involved in their own health. They work to make sure people understand their conditions and can make good choices about their care. It’s all about putting the patient first.
What does ‘patient engagement’ really mean?
Patient engagement means helping people become active partners in their healthcare. Instead of just being told what to do, patients learn to understand their needs, ask questions, and take part in decisions about their treatment. It’s like being a team with your doctor.
How does Context Media Health gather information to help patients?
They use information from many places, like what doctors record and what patients say about their health. They also do special studies and watch how people manage their health in everyday life. This helps them learn what works best.
How does technology play a part in helping patients?
Technology is super important! It helps by giving patients tools to track their health, connect with doctors, and learn more about their conditions. It also makes it easier to run clinical trials by involving patients through digital methods.
How do they figure out if their healthcare solutions are actually good?
They look at how well treatments work and if patients feel better or have better lives because of the care they receive. It’s not just about selling medicines; it’s about making sure people get real, helpful results.
What’s next for Context Media Health in patient engagement?
The future is about making patient involvement even stronger. They want to keep finding new ways to help patients be partners in their care, always trying to get better and build lasting relationships with patients and their families.