Health technology assessment, or HTA, is how we figure out if new medical stuff is actually worth it. It’s supposed to help make sure we spend our healthcare money wisely and give patients the best care. But sometimes, the old ways of doing HTA don’t quite get what’s new and exciting about certain innovations. This article looks at how we can update HTA to better support new ideas in healthcare, making sure we don’t miss out on technologies that could really help people.
Key Takeaways
- The standard health technology assessment (HTA) process can be slow to recognize and reward new innovations, often focusing too narrowly on immediate therapeutic value and cost savings.
- There’s a growing need to define innovation more clearly within HTA frameworks to encourage and support the development of new healthcare technologies.
- Tools like horizon scanning, multicriteria decision analysis (MCDA), and flexible funding mechanisms (like managed entry agreements) can help HTA better evaluate and incorporate innovation.
- Assessing non-drug technologies, such as devices and diagnostics, presents unique challenges due to differing evidence standards, highlighting the importance of real-world data.
- Moving forward, collaboration between industry and agencies, along with a unified value framework, will be vital for HTA to effectively drive innovation, especially with the rise of digital health and genomics.
Redefining Health Technology Assessment For Innovation
Health technology assessment, or HTA, has traditionally been a gatekeeper, making sure new medical stuff is safe, works well, and doesn’t cost too much. It’s done a decent job of that, but lately, there’s a feeling that the old ways aren’t quite cutting it anymore, especially when it comes to new ideas.
The Traditional HTA Framework’s Limitations
The standard HTA process often focuses heavily on whether a new treatment or device offers a clear, measurable improvement in patient health compared to what’s already available. It also looks at the cost-effectiveness, basically asking if the benefits justify the price tag. This approach makes sense for a lot of things, but it can sometimes miss the mark when it comes to truly novel technologies. Think about it: if something is brand new, it might not have a long track record of evidence yet, or its benefits might be harder to quantify in the usual ways. The system can be slow to adopt things that don’t fit neatly into existing boxes, and sometimes, innovation gets sidelined because it doesn’t immediately show a massive cost saving or a dramatic clinical win.
The Need for Explicit Innovation Criteria
Because of these limitations, there’s a growing call to make innovation a more direct part of the HTA conversation. Instead of just hoping that innovative things get picked up, we need to build specific ways to recognize and reward them. This means moving beyond just looking at therapeutic value and cost. We need to think about what makes something innovative in the first place and how we can actively encourage that. It’s about shifting HTA from being a hurdle to being a partner in bringing new solutions to patients.
Defining Innovation Beyond Therapeutic Value
So, what does ‘innovation’ really mean in this context? It’s not just about a new drug or a fancy piece of equipment. Innovation can be a new way of delivering care, a different approach to a problem, or a simple tool that makes things better for patients or doctors. It’s about looking at the bigger picture of value, not just the immediate clinical outcome or price. We need to consider things like:
- Novelty: Is this genuinely new or a significant improvement on existing approaches?
- Potential Impact: Does it have the capacity to transform care, even if the evidence is still developing?
- Patient-Centricity: Does it address unmet patient needs or improve their experience of care?
By broadening our definition, we can start to see innovation in more places and create a system that’s more open to new possibilities.
Leveraging Advanced Tools in Health Technology Assessment

So, traditional health technology assessment (HTA) has its limits, right? It often focuses too much on just the immediate cost and whether something works better than what we already have. But what about the really new stuff, the things that might change the game down the line? That’s where we need to get smarter and use some more advanced tools.
The Role of Horizon Scanning
Think of horizon scanning as an early warning system. It’s about looking ahead, way ahead, to see what’s coming down the pipeline in terms of new health technologies. This isn’t just about drugs; it includes devices, digital health tools, and even new ways of doing things in healthcare. The goal is to spot these emerging technologies before they’re fully developed and hit the market. This gives us time to prepare, understand their potential impact, and figure out how they might fit into our healthcare system. It’s like checking the weather forecast before a big trip – you want to know what to expect.
Here’s a simplified look at what horizon scanning involves:
- Information Gathering: Actively searching for new scientific publications, patent filings, conference proceedings, and industry news.
- Analysis: Evaluating the novelty, potential clinical impact, and feasibility of emerging technologies.
- Reporting: Communicating findings to decision-makers so they can plan for future adoption and assessment.
Multicriteria Decision Analysis for Broader Value
Sometimes, just looking at whether a new treatment is cheaper or more effective isn’t enough. Multicriteria Decision Analysis (MCDA) helps us consider a wider range of factors when deciding if a new technology is worth adopting. Instead of just focusing on one or two things, MCDA lets us weigh multiple aspects of value. This could include things like how innovative the technology is, its impact on patient quality of life, how easy it is to use, or even its potential to improve health equity. Different people or groups might care more about different things, and MCDA provides a structured way to bring all those perspectives together.
Let’s say we’re looking at a new diagnostic tool. We might use MCDA to consider:
- Clinical Accuracy: How well does it detect the condition?
- Patient Experience: Is it less invasive or more convenient than current methods?
- System Efficiency: Does it speed up diagnosis or reduce the need for other tests?
- Equity: Does it improve access for underserved populations?
Funding Mechanisms to Incentivize Progress
Getting new technologies into the hands of patients can be tricky. Sometimes, there isn’t enough solid evidence yet to justify a full, upfront investment. This is where creative funding mechanisms come in. Think of things like ‘coverage with evidence development’ or ‘managed entry agreements’. These approaches allow patients to access promising new technologies sooner, while still requiring more data to be collected. It’s a way to balance the need for early access with the need for robust evidence. This can encourage developers to keep innovating, knowing there’s a pathway for their technology, even if it’s not perfect on day one. It shifts the focus from a simple yes/no decision to a more dynamic process of learning and adaptation.
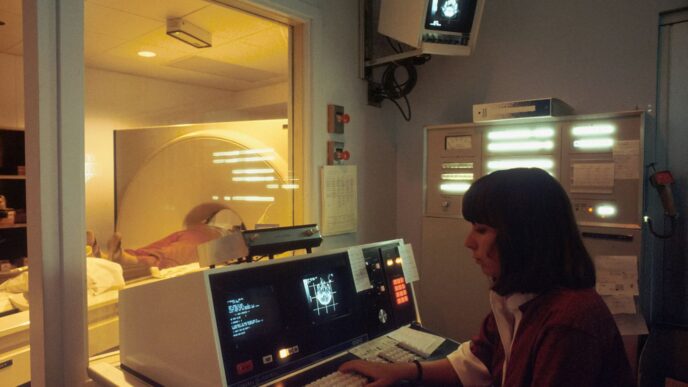
Evaluating Non-Drug Technologies
Assessing things like new medical devices, diagnostic tools, and digital health solutions presents its own set of hurdles for Health Technology Assessment (HTA). It’s not quite the same as looking at a new pill.
Challenges in Assessing Devices and Diagnostics
One big issue is the evidence we get. Clinical studies for devices are often designed to satisfy regulators, and they might build on existing knowledge about similar technologies. This means we don’t always get the kind of rigorous, head-to-head comparisons we’d ideally want, like randomized controlled trials. For diagnostics, especially new biomarker or genetic tests, the evidence can be even trickier. Sometimes we rely on indirect proof of what works, and there might not even be a clear ‘gold standard’ to compare against. This makes it tough to say definitively how good they are.
Evidence Standards for Novel Interventions
So, what kind of proof do we need? It’s a question that’s still being worked out. Traditional methods, like cost-effectiveness analyses that look at things like the Incremental Cost-Effectiveness Ratio (ICER), often miss the full picture for these non-drug innovations. Think about a digital health app – it might offer huge benefits in patient engagement or preventative care, but those advantages are hard to put a number on in a standard cost-benefit calculation. Some agencies are starting to consider other factors, like unmet patient needs or whether a technology is truly novel, to justify funding even if it doesn’t meet the usual cost-effectiveness targets. It’s about recognizing that value isn’t always just about direct cost savings.
Bridging the Evidence Gap with Real-World Data
To get a better handle on these technologies, we’re increasingly looking at real-world data. This means gathering information after a technology is already in use, seeing how it performs in everyday clinical practice. It can help fill in the gaps where traditional studies fall short. This shift towards real-world evidence is becoming more important as we try to understand the broader impact of non-drug health technologies. It allows us to see benefits that might not have been apparent in controlled trials and helps make more informed decisions about adoption and reimbursement.
Fostering Collaboration and Future Directions
Okay, so we’ve talked a lot about how health technology assessment (HTA) is changing, right? It’s not just about saying ‘yes’ or ‘no’ to new stuff anymore. A big part of this evolution is getting everyone to work together better and thinking about what’s coming next. It’s like trying to build a really complicated puzzle, and you need all the pieces and all the players to make it work.
Industry-Agency Partnerships in HTA
Honestly, the old way of doing things, where industry and the agencies assessing technologies were kind of on opposite sides, just doesn’t cut it anymore. We need these groups to actually talk to each other. Think about it: industry knows their tech inside and out, and the agencies know what the health system needs and how to evaluate things. When they team up, it can really speed things up. They can figure out what kind of evidence is actually needed before a technology is even fully developed, which saves a ton of time and money. It’s about building trust and sharing information so that when a new technology comes along, it’s already got a good foundation for assessment.
- Early engagement: Getting industry and HTA bodies talking early in the development process.
- Shared understanding: Agreeing on what constitutes good evidence for novel technologies.
- Streamlined processes: Working together to make the assessment pathway clearer and more predictable.
- Feedback loops: Creating ways for agencies to give input on development and for industry to explain their innovations.
Developing a Unified Value Framework for Innovation
This is a tricky one. Right now, everyone seems to have their own idea of what ‘value’ means, especially when it comes to innovation. Is it just about clinical outcomes? Or does it include patient experience, societal impact, or even how well it fits into existing workflows? We really need a more agreed-upon way to look at this. Having a common framework would help make decisions fairer and more consistent across different technologies and even different regions. It’s not about creating a rigid checklist, but more like a set of guiding principles that acknowledges the many facets of innovation.
| Aspect of Value | Description |
|---|---|
| Clinical Effectiveness | Does it work? Does it improve health outcomes compared to what we have now? |
| Patient Experience | How does it affect the patient’s life, comfort, and overall journey? |
| Economic Impact | What are the costs and potential savings? Is it a good use of resources? |
| Equity & Access | Does it reach everyone who needs it, or does it create new barriers? |
| Societal Benefit | What’s the broader impact on the community or public health? |
The Impact of Digital Health and Genomics
These areas are exploding, and HTA needs to keep pace. Digital health tools, like apps and AI-driven diagnostics, and advancements in genomics, like personalized medicine, are changing the game. The evidence for these can be different from traditional drugs or devices. We’re talking about data that’s constantly being updated, algorithms that learn, and genetic information that’s unique to individuals. HTA needs to figure out how to assess these dynamic and complex technologies. This means looking at things like data privacy, algorithm validation, and how to interpret real-world data that’s generated continuously. It’s a whole new ballgame, and we’re still figuring out the best way to play.
The Evolving Role of Health Technology Assessment
From Barrier to Facilitator of Innovation
Health Technology Assessment (HTA) used to be seen by many as a roadblock, a tough hurdle that new medical tools and treatments had to clear before they could reach patients. The old way of doing things often focused too much on whether something was cheaper or just a little bit better than what we already had. This made it hard for truly groundbreaking ideas to get a foot in the door, especially if they were expensive upfront or didn’t have years of data behind them. But things are changing. HTA is starting to shift from just saying ‘no’ or ‘not yet’ to actively looking for ways to help good ideas move forward. It’s becoming more about figuring out how to support innovation, not just judge it.
Informing Equitable and Efficient Health Systems
HTA’s main job is still to make sure our healthcare systems are fair and use money wisely. This means looking at who benefits from a new technology and whether it actually makes things better for everyone, not just a select few. It’s about making sure that as we bring in new treatments or devices, we’re not leaving people behind or wasting precious resources. We need to think about how these new things fit into the bigger picture of healthcare delivery.
Driving Evidence-Based Decision Making
At its heart, HTA is about making smart choices based on solid proof. It’s a process that brings together different kinds of information – like how well a treatment works, its safety, and its cost – to help leaders decide what to adopt. The goal is to make sure that the decisions made about healthcare technologies lead to the best possible outcomes for patients and the public. This means constantly looking at new evidence as it comes out and being willing to adjust our thinking. It’s a continuous cycle of learning and improving how we care for people.
Looking Ahead
So, where does all this leave us? Health technology assessment is definitely changing. It’s moving beyond just looking at price tags and basic benefits. The goal now is to really figure out how new ideas can help patients and make our healthcare systems work better. This means we need smarter ways to look at new treatments and tools, like using different decision-making methods and finding ways to fund things while we learn more. It’s not always easy, and there are still kinks to work out, but the push is on to make sure that truly helpful innovations get a fair shot. By working together and being a bit more open-minded, we can help bring the next wave of health tech to the people who need it most.