If you’re following medical device news, you know that 2025 is shaping up to be a big year for new ideas and tech in healthcare. The largest companies are flush with cash, and there’s been a flurry of deals and investments already. From smart AI tools to gadgets you can wear on your wrist, companies are racing to change how doctors and patients manage health. Some of these trends might sound futuristic, but they’re closer than you think. Here’s what’s making headlines and what to watch for as the year unfolds.
Key Takeaways
- AI is getting better at spotting diseases early, sometimes even before symptoms show up, making diagnostics much faster and more accurate.
- Wearable devices are moving beyond fitness trackers to help people and doctors keep tabs on chronic conditions and daily health.
- Robots in the operating room are becoming more common, aiming to make surgeries less invasive and help patients recover quicker.
- 3D printing is now used to make custom implants and tools tailored to each patient, speeding up recovery and improving outcomes.
- Remote monitoring and telemedicine are letting patients get care from home, which is especially helpful for those with long-term health issues or who live far from clinics.
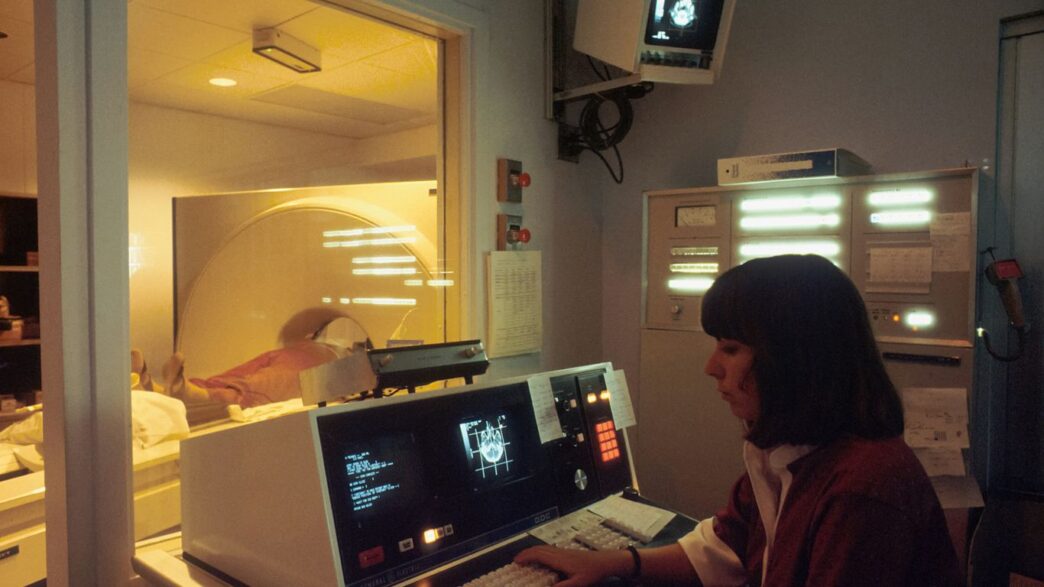
Artificial Intelligence-Powered Diagnostics
Over the past year, AI-driven diagnostics have moved from fantasy to a daily topic in med device newsrooms and doctor’s offices. Clinicians aren’t just relying on experience and best guesses anymore—machines are crunching tons of data to catch patterns that people would miss.
Here’s what’s actually changing in 2025:
- AI tools are reading medical images faster and with fewer mistakes than some specialists.
- Healthcare providers get decisions supported by smart systems that keep up-to-date with new research instantly.
- Labs and clinics are using AI to sift through piles of patient data—results, symptoms, even scanned paper records—for faster, more precise diagnoses.
A lot of this is about reducing risk and human error, but there’s more to it. These AI systems are smart enough to keep learning from each new case, which makes them more reliable each month. Hospitals are reporting shorter diagnostic times, especially for cancer and genetic diseases. Costs are dropping, too, since teams don’t need to run as many repeat tests.
Here’s a glimpse into the numbers:
| Metric | 2024 Value | Projected 2025 |
|---|---|---|
| AI market in life sciences (USD) | $2.22 billion | $3.1 billion |
| Error reduction in diagnosis (%) | 12 | 17 |
| Average workflow speed-up (%) | 18 | 23 |
AI-powered diagnostics are also moving out of city hospitals and into smaller clinics and even rural care centers. This shift brings more accurate and faster care to people who don’t live near specialists. It’s not just hype—teams on the ground are starting to trust these digital partners. It’s worth noting, this tech is still growing. Your doctor will use these tools, but their knowledge and experience still matter. If there’s one headline for AI diagnostics in 2025, it’s this: machines and humans working together are changing patient care for the better.
Wearable Health Technology
Wearable health technology isn’t just for counting steps anymore. In 2025, wearables have moved deep into the world of real medicine, not just fitness. The newest generation of devices can monitor heart rhythms, track blood sugar, and even alert users about irregular breathing—sometimes before they notice any problems themselves.
Here’s what makes wearable health tech so interesting right now:
- Constant monitoring: These devices gather health data around the clock, often catching important patterns that might be missed in a short doctor’s visit.
- Real-time alerts: Many can let you know immediately if something isn’t right, from sudden heart rate spikes to low oxygen levels.
- Remote sharing: Most wearables now connect securely to apps or health platforms, making it easy to share results with a doctor from home.
The global market for wearable medical tech is really taking off. Just look at this quick projection:
| Year | Global Wearable Medical Tech Market (USD Billion) |
|---|---|
| 2023 | 34.8 |
| 2025 | 54.7 |
| 2030 | 170.9 |
(Source: Industry forecasts, 2025)
Healthcare companies are rolling out new wearables all the time: continuous glucose monitors for people looking to keep an eye on their sugar, advanced ECG patches, even smart rings tracking temperature and sleep. There’s definitely a flip side; privacy is a worry since these gadgets collect sensitive information. Still, most people are willing to trade a little privacy for convenience, especially if it means catching something serious early. Wearable health tech is set to become even more important for people with chronic conditions, those who want to keep a closer watch on their health, or anyone looking to make smarter decisions about their daily habits.
Surgical Robotics
Surgical robots have been shaking up the operating room in ways that would’ve sounded like science fiction not long ago. 2025 looks to be the year when these machines become far more common—reliable partners for surgeons, not just fancy gadgets in high-tech hospitals. For instance, the da Vinci 5 system got the green light from the FDA in March 2024, and its full launch in 2025 means it could soon be used for most operations, except for the trickiest pediatric and heart surgeries.
Market-wise, the numbers are climbing fast:
| Year | Market Value (USD billions) | % of Surgeries with Robots |
|---|---|---|
| 2025 | 8+ | ~2% |
| 2032 (est.) | 24+ | >6% |
But right now, only about 2% of all surgeries use robots, so there’s a lot of room left to grow.
Here are a few trends taking shape:
- New players: Aside from leaders like Intuitive (the da Vinci folks), companies like Medtronic are making moves, hoping their systems (like Hugo) can chip away at the giant’s huge market share.
- Better tech in the OR: Robots now bring sharper vision, steadier hands, and even AI insights. Some robots can give real-time data or overlay digital info—making surgeons’ jobs a bit less stressful on those long, complex procedures.
- Remote surgery potential: It’s on the horizon. We’re not talking about doctors in a different country yet, but remote-assist or teleoperated surgery is inching closer each year.
This all sounds exciting, but there are still hurdles: getting enough surgeons trained, improving access for smaller hospitals, and keeping up with new rules in places like Europe. Still, people are already noticing faster recoveries and fewer complications when robots lend a hand. The bottom line—surgical robots are moving from hype to standard in more and more ORs, and it’s only just starting.
3D Printing for Personalized Medicine

3D printing isn’t just for fancy new gadgets anymore—it’s shaking up how healthcare works, too. In 2025, hospitals and clinics are using 3D printing to make custom implants, prosthetics, and even dental devices that fit each patient perfectly. That means less time spent waiting, fewer surgeries to get things just right, and a real difference in how folks heal and get back to life.
A few things are fueling this momentum:
- It’s now possible to print complex shapes that were impossible with old-school manufacturing—think tiny bone structures or unique joint replacements.
- Costs are dropping, making these personalized solutions easier for hospitals to offer without breaking the bank.
- Surgeons use 3D-printed models of organs or bones to plan tough procedures, which helps cut down on mistakes and surprises in the operating room.
Bioprinting is a wild card to watch. Lab teams are trying to print tissues and—down the road—even full organs. That’s not tomorrow’s solution for everyone, but research is moving fast, and early trials give hope for people waiting for transplants.
Here’s a quick table to show how 3D printing is showing up in medicine in 2025:
| Application | Typical Use | Expected Patient Impact |
|---|---|---|
| Custom Implants | Joint, cranial, spinal | Faster recovery, better fit |
| Dental Devices | Aligners, crowns | Quicker turnarounds |
| Prosthetics | Limbs, external supports | Improved comfort & movement |
| Surgical Planning Models | Heart, tumor models | Fewer complications |
It’s not a stretch to say that 3D printing is going to keep changing what’s possible in personalized care. If you’ve been frustrated by healthcare’s one-size-fits-all approach in the past, the future’s looking a heck of a lot more custom-made.
Remote Patient Monitoring
Remote patient monitoring (RPM) is quietly changing the way many people get healthcare. Doctors can now track vital signs and health stats in almost real time, and patients don’t have to run to the clinic for every small concern. Instead, smart devices keep tabs on things like heart rate, blood pressure, and blood sugar from home, then send that info right to the care team.
A few real-world examples of RPM tools used in 2025 include:
- Wearable ECG patches that watch for irregular heartbeats and send alerts if anything looks off.
- Blood pressure cuffs that upload your numbers to your doctor’s dashboard as soon as you use them.
- Continuous glucose monitors for people with diabetes so daily fingersticks are becoming less common.
Here’s a quick look at the impact of RPM in a typical health system:
| Benefit | 2024 Baseline | 2025 Projection |
|---|---|---|
| Hospitalizations Reduced (%) | 12 | 18 |
| Patient Satisfaction Improved (%) | 65 | 72 |
| In-person Visits Needed (%) | 100 | 78 |
RPM isn’t just about convenience—it’s also expected to keep folks healthier at home and catch issues early before they land people in the hospital. Of course, there’s still work to be done around data security and getting easy tech into everyone’s hands, especially in remote or lower-income areas. But the trend is clear: home-based monitoring is quickly becoming part of normal healthcare, and 2025 is set to see more tools, more patients, and better outcomes.
Continuous Glucose Monitoring
Continuous glucose monitoring (CGM) has moved from a highly specialized tool into something that’s almost mainstream in 2025. People with diabetes aren’t the only ones using CGMs anymore—now you’ll see athletes, health trackers, and even casual users interested in what their blood sugar is doing throughout the day. The devices have shrunk in size, gotten cheaper, and you can even find some over-the-counter models at your local pharmacy—no prescription needed.
Here’s what really stands out about where CGMs are heading:
- Real-time feedback: Modern CGMs send instant readings straight to your phone or smartwatch, so you actually see how your body responds to different foods, workouts, or stress. No more guessing or waiting for lab results.
- Better accuracy: Newer sensors last longer, stick better, and give more dependable data. Some models only need changing once every two weeks.
- Direct to consumer: Companies are skipping the middle steps—people are buying, using, and even interpreting their own glucose numbers without a doctor in the mix.
To put this shift into perspective, check this quick table showing changes in CGM access:
| Year | Prescription Required | Approximate Cost (USD) | Typical Wear Time (days) |
|---|---|---|---|
| 2020 | Yes | $200-300/month | 7-10 |
| 2025 | No (many models) | $50-120/month | 14 |
For people with diabetes, CGMs have been a game-changer for years—fewer fingerpricks, fewer scary drops or spikes, and way more info to adjust insulin (or food) on the fly. But the 2025 trend is about everyone else; the "wellness" crowd is getting into glucose tracking to try and optimize daily energy or spot triggers for tiredness. While there’s a bit of hype, there’s also data piling up that this tech can reduce diabetes-related emergencies and even help some folks catch blood sugar problems early.
The big catch? CGMs bring up some privacy worries since the data goes through apps and cloud platforms, not just to your doctor. That’s a tradeoff more people will have to think about as these sensors go fully mainstream.
Minimally Invasive Surgery

In the world of surgery, 2025 is shaping up to be all about doing more while cutting less. Minimally invasive surgery (MIS) has become the new standard for so many conditions, from hernia repair and gynecological procedures to joint replacements. Smaller incisions mean fewer complications, quicker recovery, and a whole lot less pain for patients.
Here are a few trends and facts worth watching:
- Surgical robots, like Intuitive Surgical’s da Vinci and Medtronic’s Hugo, are showing up in more operating rooms. These platforms help doctors be extremely precise—especially in tight spaces—and this means less chance of mistakes. The tech keeps getting better, too, with improved cameras and more flexible robotic arms.
- The competition is heating up. Intuitive Surgical’s da Vinci still leads the market, but Medtronic is looking to gain ground with its Hugo system. Many hospitals are holding on to their da Vinci units while watching how Hugo performs in clinical trials for new types of surgeries.
- Robotic and smart platforms are now working together with AI. You might hear about procedures where the robot not only assists with steady hands but offers real-time advice or enhanced visibility using augmented reality overlays.
Surgeons get a bit of a learning curve, but many say it pays off in the long run. Here’s a table showing the main benefits of MIS versus traditional open surgery:
| Feature | Minimally Invasive Surgery | Traditional Open Surgery |
|---|---|---|
| Incision Size | Small (0.5–1.5 cm) | Large (over 6 cm) |
| Recovery Time | 1–2 weeks | 4–8 weeks |
| Infection Rate | Lower | Higher |
| Pain | Less | More |
| Hospital Stay | Often outpatient/1-2 days | 5–7 days |
There’s a lot going on in the regulatory world, too, as authorities in the US and Europe figure out how to assess the next wave of smart surgical tools. Nobody’s saying open surgery is going away completely, but if you need an operation in 2025, MIS is more likely than ever. It’s changing the way people think about surgery—maybe not making it fun, but at least making it easier to bounce back.
Precision Medicine Solutions
Precision medicine is one of those things that sounds almost futuristic, but it’s actually changing how doctors treat us, right now. Instead of getting the exact same medication as everyone else, your treatment can be shaped by your genetics, lifestyle, or even your hometown salad preference. The idea is to move away from cookie-cutter medical care and make treatments that fit you as an individual, not just your diagnosis.
This shift is picking up speed in 2025—especially for cancer and rare diseases—because of some pretty wild advances:
- Genetic testing is way faster and cheaper, so you might find out what medicines work best for you without any guessing games.
- Doctors use AI to spot which treatments will or won’t do the trick, based on huge piles of patient data.
- There’s a push for better biomarker tests, so your blood or tissue samples reveal more than ever about what’s happening in your body.
Here’s a quick snapshot of how precision medicine trends are lining up for 2025:
| Area | Best Use Cases | More Common In 2025? |
|---|---|---|
| Cancer care | Targeted therapies | Yes |
| Rare disease drugs | Gene therapy | Yes |
| Diabetes treatment | Tailored medications | Yes |
It’s not a perfect science—insurance and cost still get in the way for lots of people. But every year, more clinics are rolling out these tools. If you have a health issue that’s tough to pin down or treat, don’t be shocked if your doctor starts talking about genetic panels or personalized care this year. It’s not science fiction anymore; it’s just medicine getting a little more personal.
Telemedicine Integration
Telemedicine has totally changed the way folks use healthcare. In 2025, these tools aren’t just for emergencies or folks in remote areas—they’re becoming a routine part of every doctor’s toolkit. It feels pretty strange at first, chatting to your doctor over video instead of sitting in a cold waiting room, but now it’s almost normal, especially since the pandemic pushed everything online. What’s really making telemedicine stick is how well it connects with modern devices and medical data, letting people track their own health from home or wherever they happen to be.
Here’s what’s making telemedicine integration work:
- Patients can schedule virtual appointments with specialists without traveling.
- Devices like smartwatches, blood sugar monitors, or portable ECGs send real-time updates right to doctors.
- Records and health updates move electronically between clinics so everyone stays on the same page.
To give you an idea of the shift, check out this short table on telemedicine adoption rates in US hospitals:
| Year | % of Hospitals Using Telemedicine |
|---|---|
| 2022 | 65% |
| 2023 | 74% |
| 2024 | 82% |
| 2025 | 89% (projected) |
It’s not just about video calls. Whether it’s hospital-at-home care for chronic conditions, sending medication reminders, or using devices that keep tabs on breathing or heart rhythms around the clock, telemedicine is filling gaps that traditional visits can’t. Of course, the tech boom means there are real concerns about making sure patient data is safe from hackers, but that’s getting plenty of attention too. If the trend keeps up, no one will be surprised if telemedicine appointments outnumber office visits in a few years. And honestly, who misses sitting in those old waiting rooms anyway?
Next-Generation Spinal Implants
In 2025, spinal implants are starting to look a lot different than they did even just a few years ago. New designs and materials are making surgeries less invasive and outcomes a lot more promising for patients. These next-generation implants ditch traditional bulky hardware for smaller, smarter, and sometimes even 3D-printed solutions.
Here’s what’s really changing in spinal implants:
- Porous Implants: These allow for better integration with bone, meaning the body accepts the implant more easily and healing time drops.
- No-Screw Fusion: Some new devices skip using screws, aiming for faster and simpler procedures with less chance of long-term pain.
- Smart Materials: There’s a push toward implants that aren’t just metal but a blend of materials, or even those that slowly dissolve as the body heals.
A quick look at some key improvements:
| Feature | 2022 Technology | 2025 Advancements |
|---|---|---|
| Surgery Recovery Time | 6-12 weeks | 3-6 weeks |
| Need for Revision | Up to 20% | Projected 10% or lower |
| Integration Rate | ~60% | Over 80% (expected) |
Surgeons aren’t the only fans. People living with chronic spine issues say recovery is smoother and pain less intense. While it’s still early days for some of the more experimental implants, all signs point to these advances sticking around—and getting even better with time.
Conclusion
So, looking ahead to 2025, it’s clear that the medical device world isn’t slowing down. Big companies are making moves, startups are popping up with fresh ideas, and there’s a lot of money flowing into new tech. AI, robotics, and personalized medicine are all getting more attention, and we’re seeing more devices that help people manage their health outside of hospitals. At the same time, companies are thinking about things like health equity and sustainability, which is a good sign. There’s still a lot of uncertainty—regulations, the economy, and global events can all shake things up—but the drive to improve healthcare keeps pushing the industry forward. If you’re following medtech, 2025 should be an interesting year to watch.