So, there’s this new tech called augmented reality, or AR for short. It’s basically like layering computer stuff onto what you see in real life, usually through a phone or special glasses. Turns out, it’s starting to change how we teach doctors and nurses. Instead of just reading books or looking at flat pictures, students can now interact with 3D models of the human body or practice tricky procedures in a more hands-on way. This article is going to look at how augmented reality in medical education is making a difference, from helping students learn anatomy better to practicing surgery, and what the future might hold.
Key Takeaways
- Augmented reality (AR) mixes digital information with the real world, offering new ways to learn in medicine.
- AR helps medical students get a better grasp of anatomy and how the body works through interactive 3D models.
- Students can practice skills, like surgery, in a safe, simulated environment using AR, improving their practical abilities.
- AR technology has applications beyond training, including patient care, physical therapy, and making education more accessible.
- While AR has great potential, challenges like cost and the need for more research need to be addressed for wider use in medical training.
Augmented Reality’s Role in Medical Education
Augmented reality, or AR, is basically a way to layer digital stuff onto what you’re already seeing in the real world. Think of it like adding a digital sticker or information bubble to your view of a patient or an anatomical model. It’s not like virtual reality, where you’re completely in a made-up world. AR keeps you grounded in reality but adds digital elements, which can be anything from 3D models to real-time data. This technology is changing how we learn, especially in fields like medicine.
Understanding Augmented Reality in Healthcare
AR in healthcare means using digital overlays to help doctors, nurses, and students. It’s a flexible tool that can show you things you wouldn’t normally see, like the internal structure of a body part or the flow of blood. Because it only adds to reality, you can control how much digital information is presented, making it a really tailored learning experience. This is different from virtual reality (VR), which creates a whole new digital environment. AR and VR are actually on a spectrum of what’s called mixed reality, a concept that’s been around for a while.
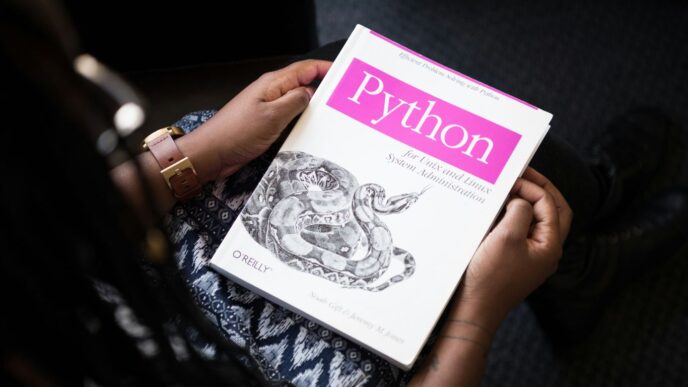
The Evolution of AR in Medical Training
AR is a fast-moving technology, and its use in medical training is growing. It’s great for showing complex information in a more engaging way. Students often find AR tools fun and interesting to use, much like popular AR games. This technology can improve how information is presented and how our senses are used in learning, which are key ideas in how people learn best. Since many students are already comfortable with tablets and smartphones, picking up AR tools feels natural. Plus, using devices they already own means they can learn at their own pace.
AR Versus Virtual Reality in Learning
When comparing AR and VR for learning, there are some key differences. AR adds digital elements to your real surroundings, often through a headset or a tablet. This means you’re still aware of your actual environment. VR, on the other hand, completely immerses you in a digital world, blocking out reality. For medical training, AR has an advantage because it’s less likely to cause side effects like dizziness or headaches that some people experience with VR. Studies have shown that AR programs on tablets can lead to similar learning results as VR programs, but with fewer discomforts. This makes AR a more accessible option for many students and training scenarios.
Enhancing Medical Student Learning Outcomes

Augmented reality (AR) is really changing how medical students learn, going beyond just reading books or looking at static diagrams. It’s about making the learning process more active and, frankly, more effective.
Deepening Knowledge and Anatomical Understanding
Remember trying to learn anatomy from textbooks? It was tough, right? AR lets students interact with 3D anatomical models that float right in front of them. You can spin them around, zoom in, and see how everything fits together in a way that flat images just can’t replicate. This hands-on digital approach helps solidify what they’re learning about the human body, making complex structures easier to grasp. It’s like having a virtual cadaver you can explore from every angle, without any of the limitations of traditional methods.
Developing Practical and Surgical Skills
Medicine isn’t just about knowing things; it’s about doing things. AR is a game-changer for practicing procedures. Students can use AR to simulate surgeries or patient examinations in a safe space. This means they can try things out, make mistakes, and learn from them without any risk to actual patients. Think about practicing a tricky surgical step over and over until it feels natural. AR makes that possible, building confidence and competence before they even step into a real operating room or clinic. It bridges the gap between theoretical knowledge and hands-on ability.
Cultivating Essential Social and Communication Skills
Doctors don’t just treat bodies; they treat people. AR can also help students practice how they interact with patients and colleagues. Imagine AR scenarios where students have to explain a diagnosis to a virtual patient or work through a medical emergency with a simulated team. These simulations provide a controlled environment to hone communication, teamwork, and decision-making skills. Practicing these soft skills in a realistic, yet consequence-free, setting is incredibly important for future patient care. It prepares them for the complex human interactions they’ll face daily.
Transformative AR Applications in Medical Training
It’s pretty wild how much technology is changing how we learn medicine these days. Forget just staring at textbooks; augmented reality is stepping in to make things way more hands-on, even when you’re not actually in front of a patient or in an operating room. This stuff is really starting to change the game.
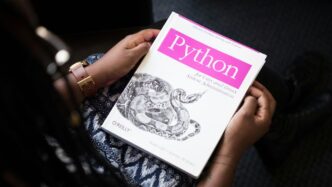
Interactive Anatomical Models with HoloHuman
Imagine being able to pull up a 3D model of the human body, right there in front of you, and being able to walk around it, zoom in, and see every single bone, muscle, and organ. That’s basically what HoloHuman does. It lets you interact with these detailed holographic anatomy models, both male and female. You can see all the parts labeled, and it doesn’t matter where you are. It’s like having a super-detailed anatomy atlas that you can actually touch and manipulate, which is a big step up from flat diagrams.
Simulated Patient Encounters with HoloPatient
This is where things get really interesting for practicing those diagnostic skills. HoloPatient lets you interact with virtual patients who have all sorts of symptoms. You can assess them, ask questions, and even see their vital signs in real-time. It’s designed to mimic real patient interactions, giving students a safe space to practice their assessment and diagnosis skills without any real-world consequences. They’ve got a bunch of different patient scenarios, so you can get a feel for a variety of conditions.
Immersive Surgical Simulation with OculAR SIM
For anyone looking to get into surgery, OculAR SIM is a pretty neat tool. Developed by Deakin University, it lets you interact with virtual humans and their anatomy in a simulated environment. This isn’t just about looking; it’s about practicing procedures. Think about learning how to perform a tricky surgery. With OculAR SIM, you can get a feel for the movements, the tools, and the steps involved. It’s a way to build confidence and muscle memory before you’re ever in a real operating room.
Augmented Reality in Surgical Procedures
When we talk about AR in medicine, surgery is a big area where it’s really starting to show its worth. It’s not just about training anymore; it’s about helping surgeons do their jobs better, right there in the operating room.
Improving Navigation and Visualization in Surgery
Think about complex surgeries. Surgeons often need to look at multiple screens, like CT scans or MRIs, while also keeping their eyes on the patient. This can be tricky and take their focus away. AR changes that. It can overlay patient-specific 3D models, built from scans, directly onto the surgeon’s view of the patient. This means they can see internal structures, like blood vessels or tumors, without looking away from the actual surgical site. It’s like having an X-ray vision that’s perfectly aligned with what they’re seeing.
Enhancing Precision in Spinal and Neurosurgery
Procedures involving the spine and brain are incredibly delicate. Even a small misstep can have serious consequences. AR tools are proving really helpful here. For spinal surgeries, AR can guide the surgeon, showing them exactly where to place screws or make incisions based on pre-operative imaging. In neurosurgery, it can provide a detailed 3D view of the brain and skull, helping surgeons map out the best approach to remove tumors or treat other conditions with more confidence. This real-time visual guidance is a game-changer for accuracy.
Training for Complex Procedures like ECMO Cannulation
Learning to perform highly specialized procedures can be tough. Take extracorporeal membrane oxygenation (ECMO) cannulation, for example. It’s a life-support technique that requires a lot of skill. Studies have shown that using AR for training this specific procedure leads to better learning outcomes and fewer mistakes compared to traditional methods. Trainees can practice steps, see virtual overlays of correct instrument placement, and get immediate feedback, all in a safe, simulated environment before they ever touch a real patient.
The Impact of Augmented Reality on Patient Care
Augmented reality (AR) isn’t just for training medical students; it’s starting to make a real difference in how patients are treated and cared for. Think about physical therapy, for instance. AR can project targets on the floor to help guide patients through exercises, making sure they move their limbs correctly. It also gives therapists data to see how well someone is progressing, which is pretty neat.
AR Applications in Physical Therapy Rehabilitation
AR is changing the game for rehabilitation. Instead of just following verbal instructions, patients can see visual cues right in front of them. This could be anything from guiding a patient’s steps on a marked path to showing them the exact angle to move a joint. This kind of interactive feedback can make therapy more engaging and effective. Plus, the data collected can help therapists fine-tune treatment plans.
Supporting Patient Monitoring and Surgical Preparation
Beyond therapy, AR has potential in keeping an eye on patients and getting them ready for surgery. Imagine a patient recovering at home. AR could overlay information on a surgical wound, allowing a remote nurse or doctor to check on it without an in-person visit. This kind of remote assistance can be a lifesaver, especially for people in rural areas or during times when in-person visits are tricky. It’s also been shown to reduce anxiety in kids before surgery, which is a big win [43e2].
Potential for Remote Learning and Accessibility
One of the most exciting parts of AR in patient care is its ability to bridge distances. Telemedicine gets a serious upgrade with AR. A specialist anywhere in the world could guide a local nurse through a procedure or diagnosis by annotating what they see in real-time. This means patients can get expert help no matter where they are. It also opens doors for remote education, letting students watch and even interact with live procedures streamed through AR headsets. This makes specialized knowledge more accessible than ever before.
Addressing Challenges and Future Directions
Even with all the cool stuff augmented reality can do for medical training, it’s not exactly a walk in the park to get it everywhere. One of the big headaches is the price tag. Developing these interactive AR programs costs a pretty penny, and let’s be honest, schools often don’t have endless piles of cash lying around. Plus, you need specific hardware, which adds to the expense and can be a barrier for students who don’t have access to it. It’s a real challenge to make sure everyone gets a fair shot at using these tools, no matter their background or financial situation.
Overcoming Barriers to AR Adoption
Getting AR into medical schools isn’t just about the money, though. There’s also the issue of getting everyone on board. Teachers need to be trained on how to use the tech effectively, and sometimes there’s just a general resistance to changing how things have always been done. Think about it: switching from a textbook to a holographic heart model is a big shift. We need to make sure the technology is user-friendly and that educators see the real benefits. It’s also important to remember that while digital learning is great, we don’t want students feeling isolated. Finding ways for AR to encourage collaboration, like having multiple students interact with the same AR model, is key.
The Need for Further Research and Evaluation
While we’ve seen some really promising results from AR in medical training, there’s still a lot we don’t know for sure. Most of the studies so far have looked at whether the technology is feasible and if it seems like a good idea to students and teachers. That’s a good start, but we really need more research that directly compares AR training to traditional methods. We need to figure out if AR actually leads to better patient outcomes down the line. For example, a study looking at how well surgeons perform after AR-assisted training versus standard training would be super helpful. We need to collect more data on how these programs impact actual learning and skill development.
Fostering Collaboration for AR Innovation
To really push AR forward in medical education, we need everyone to work together. Tech companies, medical schools, researchers, and even students need to be part of the conversation. This collaboration can help make sure the AR tools being developed actually meet the needs of educators and students. It can also help share the costs and resources needed to create and implement these programs. Imagine if different universities pooled their resources to develop a shared AR anatomy library – that would be a game-changer. The future of AR in medicine depends on us building these bridges and sharing knowledge.
Wrapping It Up
So, it’s pretty clear that augmented reality is changing the game for how we train future doctors and nurses. It’s not just about looking at screens anymore; it’s about actually interacting with complex information in a way that feels more real. From dissecting virtual bodies to practicing tricky surgeries without any risk, AR is giving students a much better grasp of what they need to know and do. Plus, with everything going digital these days, especially after the pandemic, AR fits right in. While there are still some hurdles to jump, like making the tech more affordable and doing more studies to prove its long-term impact, the direction is obvious. AR is here to stay and will likely become a standard part of medical education, helping to shape a new generation of healthcare professionals who are better prepared than ever before.
Frequently Asked Questions
What exactly is augmented reality (AR) and how is it used in medicine?
Augmented reality, or AR, is like adding a digital layer to the real world you see. Imagine wearing special glasses or looking through a tablet that shows you extra information or 3D models right in front of you, mixed with what’s actually there. In medicine, this helps students learn about the body by seeing virtual organs or bones appear on a real person or mannequin. It’s also used in surgery to guide doctors by showing them important details on a screen or through special eyewear.
How does AR help medical students learn better than old methods?
AR makes learning more engaging and easier to understand. Instead of just looking at flat pictures in a book, students can interact with 3D models of the human body, seeing how different parts work together. This hands-on approach helps them remember things better and understand complex topics, like how diseases affect the body, in a more visual and interactive way.
Can AR really help students practice difficult medical skills?
Yes, AR is great for practicing skills without real risk. For example, students can use AR to simulate surgeries, learning the steps and techniques needed. This allows them to build confidence and get the feel for procedures in a safe environment before they ever have to perform them on a real patient. It’s like practicing a video game before playing the real match.
What’s the difference between AR and VR in training?
Think of AR as adding digital things to your real world, while VR completely replaces your real world with a digital one. With AR, you still see your surroundings, but with added digital info. With VR, you’re fully immersed in a computer-generated world. For medical training, AR is often preferred because it lets students interact with real objects or people while seeing digital guides or information.
Are there any real AR tools used in medical schools now?
Absolutely! There are several exciting AR tools being used. For instance, HoloHuman lets students explore detailed 3D models of the human body, HoloPatient lets them practice diagnosing virtual patients with different symptoms, and OculAR SIM helps train students on anatomy and surgical procedures by overlaying digital information onto real-world views.
What are the challenges of using AR in medical education?
While AR is amazing, there are a few hurdles. Sometimes the technology can be expensive, and schools need to figure out how to afford it and train teachers to use it effectively. We also need more studies to prove exactly how much it improves learning in the long run. Making sure everyone can access and use these tools is also important for the future.