Ever wonder what keeps your blood from just sloshing around everywhere? It’s a bit more complex than just a pump. One of the key players in this whole system is something called osmotic pressure. You might have heard of osmosis, like when you put raisins in water and they swell up. Well, blood has its own version of this, and it’s super important for keeping things balanced. This article is going to break down the osmotic pressure of blood, why it matters, and what happens when it goes a little haywire.
Key Takeaways
- Osmotic pressure is the force that pulls water across a membrane, driven by differences in solute concentration.
- The osmotic pressure of blood is mainly due to the proteins, like albumin, dissolved in the plasma.
- This pressure helps keep fluid inside your blood vessels, preventing it from leaking out into your tissues.
- When blood osmotic pressure is too low, fluid can build up in tissues, causing swelling (edema).
- Understanding and monitoring blood osmotic pressure is important for doctors, especially when treating patients with certain illnesses or giving IV fluids.
Understanding Blood Osmotic Pressure
So, what exactly is osmotic pressure, and why should we care about it when it comes to our blood? Think of it as a sort of invisible tug-of-war happening at a microscopic level within your body. It’s all about how water moves around, and it’s pretty important for keeping things balanced.
Defining Osmotic Pressure
At its core, osmotic pressure is the force that pulls water across a special kind of barrier, called a semipermeable membrane. Imagine you have a solution with a lot of stuff dissolved in it (like salt or sugar) on one side of this membrane, and a solution with less stuff on the other. Water naturally wants to move from the side with less dissolved stuff to the side with more, trying to even things out. Osmotic pressure is the amount of pressure needed to stop that water movement from happening. It’s essentially a measure of the tendency of a solvent to move into a solution because of the solute concentration.
The Osmotic Pressure of Blood
Now, let’s bring this concept to blood. Your blood isn’t just water; it’s packed with all sorts of things – salts, sugars, and importantly, proteins. These dissolved substances are the "solutes" in our osmotic pressure equation. The concentration of these solutes in your blood plasma creates the osmotic pressure of your blood. It’s this pressure that helps keep the right amount of fluid inside your blood vessels and prevents it from leaking out too much into the surrounding tissues.
Normal Blood Osmotic Pressure Values
When everything is working as it should, your blood has a specific osmotic pressure. While it can fluctuate a bit, a typical value for blood osmotic pressure at normal body temperature (around 37°C or 98.6°F) is roughly 8.21 atmospheres (atm). That’s a pretty significant pressure! This value is largely influenced by the concentration of various solutes, with plasma proteins, especially albumin, playing a starring role.
Here’s a quick look at what contributes:
- Plasma Proteins: These are big players. Because they’re mostly too large to easily cross the blood vessel walls, they tend to stay in the blood, drawing water with them.
- Electrolytes: Things like sodium and chloride ions are also major contributors to the overall osmotic pressure.
- Other Solutes: Glucose and urea also add to the mix, though their impact is generally less than that of proteins and electrolytes.
Understanding these basic ideas sets the stage for why osmotic pressure is so vital for our health.
The Mechanism of Osmosis in Blood
Solvent Movement Across Membranes
So, how does osmosis actually work in our blood? Think of it like a busy highway where water molecules are the cars and the dissolved stuff – like salts and proteins – are the other vehicles. Osmosis is basically the process where water moves across a barrier, called a semipermeable membrane, from an area where there’s less ‘stuff’ dissolved to an area where there’s more ‘stuff’ dissolved. It’s like water trying to even things out. This net movement of water is driven by the difference in solute concentration on either side of the membrane. In our bodies, these membranes are found all over the place, especially around our cells and within our blood vessels.
The Role of Semipermeable Membranes
These semipermeable membranes are pretty neat. They’re like a bouncer at a club, letting some things through while blocking others. In the context of blood, these membranes allow water molecules to pass freely but are much more selective about what dissolved substances, or solutes, can cross. This selective nature is what allows for osmotic pressure to build up. If everything could just zip across the membrane, there wouldn’t be any pressure difference. But because water can move and many solutes can’t (or move much slower), a pressure gradient forms, pushing water towards the side with a higher solute concentration.
Osmotic Pressure Within Capillaries
Now, let’s talk about what happens inside our tiny blood vessels, the capillaries. These are where the real action happens when it comes to exchanging fluids with our tissues. The blood inside the capillaries has a certain concentration of solutes, mainly proteins like albumin and various ions. The fluid outside the capillaries, in the surrounding tissues, has a different concentration. The semipermeable membrane here is the capillary wall itself. Osmotic pressure works to pull water from the tissue fluid back into the capillaries, helping to maintain fluid balance. It’s a constant push and pull between osmotic pressure, which tries to draw water in, and hydrostatic pressure (the pressure from blood flow), which tries to push water out. Getting this balance right is super important for keeping our tissues from swelling up like balloons.
Key Determinants of Blood Osmotic Pressure
So, what actually makes blood osmotic pressure tick? It’s not just one thing, but a few players working together. Think of it like a team sport where everyone has a role.
The Significance of Plasma Proteins
This is a big one. Plasma proteins, especially albumin, are like the main anchors for osmotic pressure in your blood. They’re too big to easily slip out of your blood vessels, so they hang out in the plasma. Because they’re there in higher concentrations than in the surrounding tissues, they pull water towards them. This pulling force is what we call colloid osmotic pressure, and it’s super important for keeping fluid inside your blood vessels. Without enough of these proteins, fluid can start to leak out, leading to swelling.
Influence of Ion Concentrations
While proteins get a lot of the spotlight, the tiny charged particles, or ions, in your blood also contribute. Things like sodium (Na+) and chloride (Cl-) are major players here. They’re constantly moving around, and their concentration differences across membranes can create osmotic pressure. However, because they can move more freely between your blood and tissues compared to proteins, their effect on overall blood osmotic pressure is a bit different. They’re more about the immediate balance, while proteins have a more sustained pull.
Impact of Temperature and Hydration
Your body’s temperature and how hydrated you are can also tweak blood osmotic pressure. When you’re dehydrated, your blood becomes more concentrated with solutes, which naturally increases osmotic pressure. On the flip side, if you drink a ton of water, your blood can become more diluted, lowering the osmotic pressure. Temperature, while usually stable in a healthy body, can technically affect how solutes behave and move, but in everyday physiological terms, hydration levels are the more dynamic factor here.
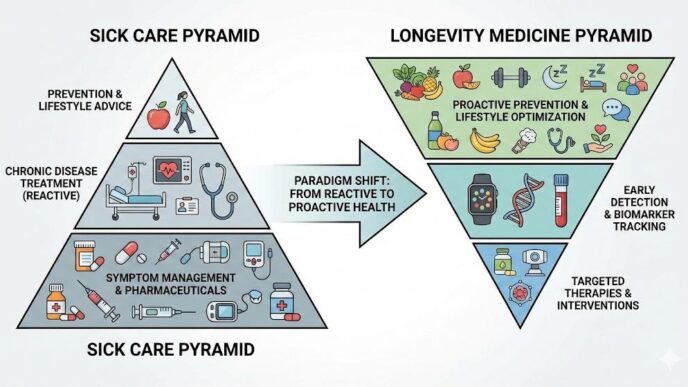
Clinical Implications of Osmotic Pressure Imbalances
So, what happens when the osmotic pressure in our blood goes a bit haywire? It turns out, it’s not just some abstract science concept; it has real, tangible effects on our bodies. When the balance is off, fluid can start to go where it shouldn’t, and that’s where problems begin.
Edema and Fluid Accumulation
Think of your blood vessels like tiny highways for fluid. Osmotic pressure is like the traffic cop, making sure fluid stays mostly inside the vessels. But if that pressure drops too low, the cop is basically asleep at the wheel. Fluid then starts to leak out into the surrounding tissues. This buildup is what we call edema, and it’s why you might see swelling, especially in your legs and feet. It’s your body’s way of showing that the fluid balance is out of whack. This can happen for a few reasons, but a common one is when there aren’t enough proteins in the blood to hold onto that fluid.
Hypoalbuminemia and Its Effects
Speaking of proteins, albumin is a big player in keeping our blood osmotic pressure where it needs to be. It’s like a sponge, attracting water back into the blood vessels. When levels of albumin drop – a condition called hypoalbuminemia – the blood’s ability to pull water back in is weakened. This directly contributes to that fluid leakage we just talked about, leading to edema. It’s a domino effect; low albumin means lower osmotic pressure, which means fluid escaping the blood vessels. This can be a sign of liver disease, kidney problems, or malnutrition, so it’s something doctors look out for.
Intravenous Fluid Therapy Considerations
When someone needs fluids given through an IV, understanding osmotic pressure is super important. Doctors and nurses have to choose the right kind of fluid. If they give a fluid that has a much lower osmotic pressure than the blood (hypotonic), it can cause water to rush into the body’s cells, potentially making them swell and even burst. On the flip side, giving a fluid with a much higher osmotic pressure (hypertonic) can pull too much water out of the cells and into the bloodstream, which can also cause problems. It’s all about matching the fluid’s concentration to the body’s needs to maintain that delicate balance. They’re essentially trying to mimic the body’s natural osmotic pressure to help restore fluid balance without causing further issues. It’s a careful balancing act, really.
Measuring and Evaluating Blood Osmotic Pressure

So, how do we actually figure out what the osmotic pressure of blood is? It’s not like you can just stick a thermometer in there and get a reading. There are a few ways to go about it, some more direct than others.
Calculating Osmotic Pressure
We can estimate blood osmotic pressure using formulas, kind of like doing a math problem. The Van’t Hoff equation is a common one. It takes into account the concentration of different solutes in the blood plasma. Think of it like this: the more stuff dissolved in the water, the more pressure it exerts. However, this calculation can get a bit tricky in real-life situations. Proteins, for instance, don’t always behave predictably, and their interactions can complicate things. So, while calculations give us a ballpark figure, they aren’t always perfectly accurate, especially when someone isn’t feeling well.
Direct Measurement Techniques
Sometimes, you just need to measure it straight up. One method involves using special wicks that soak up fluid from the tissues around blood vessels. These wicks are pre-treated with different solutions. By seeing how the fluid in the wick changes, doctors can get a good idea of the osmotic pressure in the surrounding interstitial fluid, which is closely related to blood’s pressure. It’s a bit like a sponge test, but way more scientific. These direct methods are often used when the calculated values just don’t seem right or when a really precise number is needed for treatment.
Interpreting Laboratory Tests
Beyond direct measurements, a lot of information about osmotic pressure comes from standard blood tests. When a lab checks your blood, they often measure things like protein levels, especially albumin. Since albumin is a major player in keeping water in the blood vessels, low albumin levels usually mean lower osmotic pressure. They also look at electrolyte levels, like sodium and chloride, because these ions also contribute to the overall osmotic pressure. So, by looking at a panel of lab results, doctors can piece together a picture of your blood’s osmotic pressure and how it might be affecting your body. It’s like putting together puzzle pieces to understand the whole situation.
Comparing Osmotic and Hydrostatic Forces
Blood vs. Interstitial Fluid Osmotic Pressure
So, we’ve talked about osmotic pressure and how it works in the blood. But it’s not just about the blood itself; it’s also about how it interacts with the fluid surrounding our tissues, called interstitial fluid. Think of it like this: your blood vessels are like tiny highways, and the interstitial fluid is the landscape next to them. The osmotic pressure inside the blood vessels is generally higher than in the interstitial fluid. This difference is mainly because of the proteins, especially albumin, that are floating around in your blood. These proteins are too big to easily slip out of the blood vessels, so they hang out inside, creating a sort of ‘pull’ for water. The interstitial fluid, on the other hand, has way fewer proteins. This means water tends to be drawn from the interstitial fluid into the blood vessels because of that higher protein concentration inside.
Osmotic Pressure vs. Hydrostatic Pressure
Now, let’s bring in another player: hydrostatic pressure. If osmotic pressure is like a gentle pull, hydrostatic pressure is more like a push. It’s the force exerted by the blood against the walls of the blood vessels, kind of like the pressure from water pushing against the sides of a hose. At the capillary level, these two forces are constantly working against each other. Hydrostatic pressure tries to push fluid out of the capillaries and into the surrounding tissues. Meanwhile, the osmotic pressure (mostly from those proteins we talked about) tries to pull fluid back into the capillaries. It’s a delicate balancing act.
Here’s a quick rundown:
- Hydrostatic Pressure: Pushes fluid out of blood vessels.
- Osmotic Pressure (Colloid Osmotic Pressure): Pulls fluid into blood vessels (mainly due to proteins).
Dynamics in Normal vs. Pathological States
In a healthy body, this push-and-pull system works pretty smoothly. At one end of a capillary (the arterial end), hydrostatic pressure is usually a bit higher, so some fluid and small solutes leave the blood to nourish the tissues. As the blood moves along the capillary to the venous end, hydrostatic pressure drops, and the osmotic pressure takes over, drawing most of that fluid back into the bloodstream. The little bit of fluid that doesn’t get reabsorbed is picked up by the lymphatic system. It’s a really efficient way to keep things balanced.
But what happens when things go wrong? If, for example, someone has a condition where their body isn’t making enough albumin (like in severe liver disease or kidney problems), the osmotic pressure inside the blood vessels drops. Suddenly, there isn’t enough ‘pull’ to bring fluid back in. This can lead to fluid building up in the tissues, causing swelling, a condition known as edema. On the flip side, if hydrostatic pressure gets too high (like in heart failure), more fluid might be pushed out than can be pulled back in, also leading to fluid accumulation.
Wrapping It Up
So, there you have it. Blood osmotic pressure isn’t just some fancy science term; it’s a really big deal for keeping our bodies running smoothly. It’s all about that delicate balance, mostly thanks to proteins like albumin, pulling water where it needs to go. When this balance gets thrown off, things like swelling can happen, which is why doctors pay attention to it. Understanding this pressure helps them figure out what’s going on and how to help. It’s a pretty neat example of how complex systems in our bodies work together, even when we don’t think about it.