Lately, there’s been a lot buzzing about athenahealth, especially with all the new tech they’re rolling out. It seems like they’re really pushing to make things easier for doctors’ offices and hospitals, particularly when it comes to the tricky business of billing and managing patient records. We’ve been seeing a lot of athenahealth in the news lately, and it looks like they’re focusing hard on using things like AI to cut down on the paperwork and headaches that come with running a practice. Let’s take a look at what’s new and what it means for healthcare providers.
Key Takeaways
- Athenahealth is putting a big emphasis on AI to help practices manage their operations and billing more smoothly, aiming to cut down on a lot of the manual work.
- The athenahealth network connects a lot of providers, making it easier to share patient information and get a clearer picture for making patient care decisions.
- They’re working on making the whole billing process faster and more accurate using smart technology, which should help practices get paid quicker.
- New features are being added to their main platform, athenaOne, with a focus on using AI to reduce the time staff spend on administrative tasks.
- Athenahealth is also highlighting its commitment to helping customers succeed, especially with the shift towards value-based care, and they’re building a community for users to connect.
Athenahealth’s AI-Powered Innovations
It feels like artificial intelligence is everywhere these days, and healthcare is no exception. Athenahealth is really leaning into AI, especially with its athenaOne platform. They’re not just adding a few AI features; they’re building them right into the core of their system to make things smoother for practices and for managing money.
Streamlining Practice and Revenue Cycle Management with AI
Think about all the paperwork and back-and-forth that goes into running a medical practice. Athenahealth is using AI to cut down on a lot of that. They’re aiming to reduce the administrative tasks for doctors’ offices by more than half. This means less time spent on things like checking insurance details or figuring out why a claim was denied, and more time for patient care. The goal is to make the whole process of getting paid faster and easier.
AI-Native Features for Enhanced Efficiency
What’s really interesting is that Athenahealth is developing AI features that are "AI-native." This means the AI is a fundamental part of how the system works, not just an add-on. They’re using AI to look at billions of claims and payer rules to automate tasks that used to require a person. Some of these new features include:
- Automated Insurance Selection: The system figures out the right insurance to bill automatically.
- AI Payer Portal Agents: These agents can interact with insurance company websites to get information or submit things.
- Waitlist Scheduling: AI helps manage patient waitlists more effectively.
- Automated Denial Advice: When a claim is denied, AI helps figure out why and suggests how to fix it.
This approach, built on a cloud-based system, allows for quick updates and improvements. It’s like having a system that learns and gets better over time, helping practices stay on top of changes in healthcare rules and insurance policies without constant manual effort.
Transformative Leap in Reducing Workload
Paul Brient, Chief Product and Operations Officer at athenahealth, mentioned that these AI advancements, combined with their years of experience, are leading to a big change in how much work their customers have to do. They’re seeing near 99% clean claim rates, which means claims are submitted correctly the first time, leading to quicker payments. This isn’t just a small tweak; it’s a significant shift aimed at making the financial side of healthcare less of a headache for providers.
The Athenahealth Network Advantage
Think of the Athenahealth Network as the biggest digital highway in healthcare. It’s where information travels fast and efficiently between more than 160,000 providers. This isn’t just about sending data back and forth; it’s about making that data useful right when you need it.
Open Connectivity for Enhanced Care Delivery
The core idea here is making it easy for different healthcare systems to talk to each other. When patient information can flow freely, doctors and staff can make better decisions. It helps with everything from scheduling appointments to managing patient records and getting paid. This network connects a huge number of healthcare organizations, creating a more unified system.
Personalized Interoperability for Informed Decisions
It’s one thing to have data, it’s another to have the right data surfaced in a way that makes sense for your daily work. Athenahealth takes data from across its vast network and tailors it to fit into your existing workflows. This means when you’re looking at a patient’s chart, you might see relevant information from their previous visits, even if they were at a different facility. This curated data helps you understand the full picture.
Data-Driven Insights for Practice Performance
Ever wonder how your practice stacks up against others? The Athenahealth Network provides insights based on data from similar practices. This can highlight areas where you might be doing great and areas where there’s room for improvement, especially when it comes to financial performance. It’s like having a helpful advisor who can point out trends you might have missed.
The network’s ability to share and process information in near real-time is a big deal. It means less time spent hunting for patient history and more time focused on care. Plus, the system updates itself, so you’re always working with the latest technology without a fuss.
Here’s a quick look at some numbers:
| Metric | Quantity |
|---|---|
| Providers on the Network | 160,000+ |
| Patient Records Migrated | 158 Million |
| Active Users in Community | 44,000+ |
Transforming Revenue Cycle Management
AI-Driven Automation in Billing
Remember the days of mountains of paperwork and endless manual data entry for medical billing? It feels like a lifetime ago, doesn’t it? Athenahealth is really changing that game with AI. They’re using artificial intelligence to speed up things like checking claims, making sure codes are right, and even chasing down payments for rejected claims. This means less time spent by staff on repetitive tasks, freeing them up for more important work. Practices using AI-powered billing are seeing fewer mistakes and getting paid faster. It’s a big shift from how things used to be done.
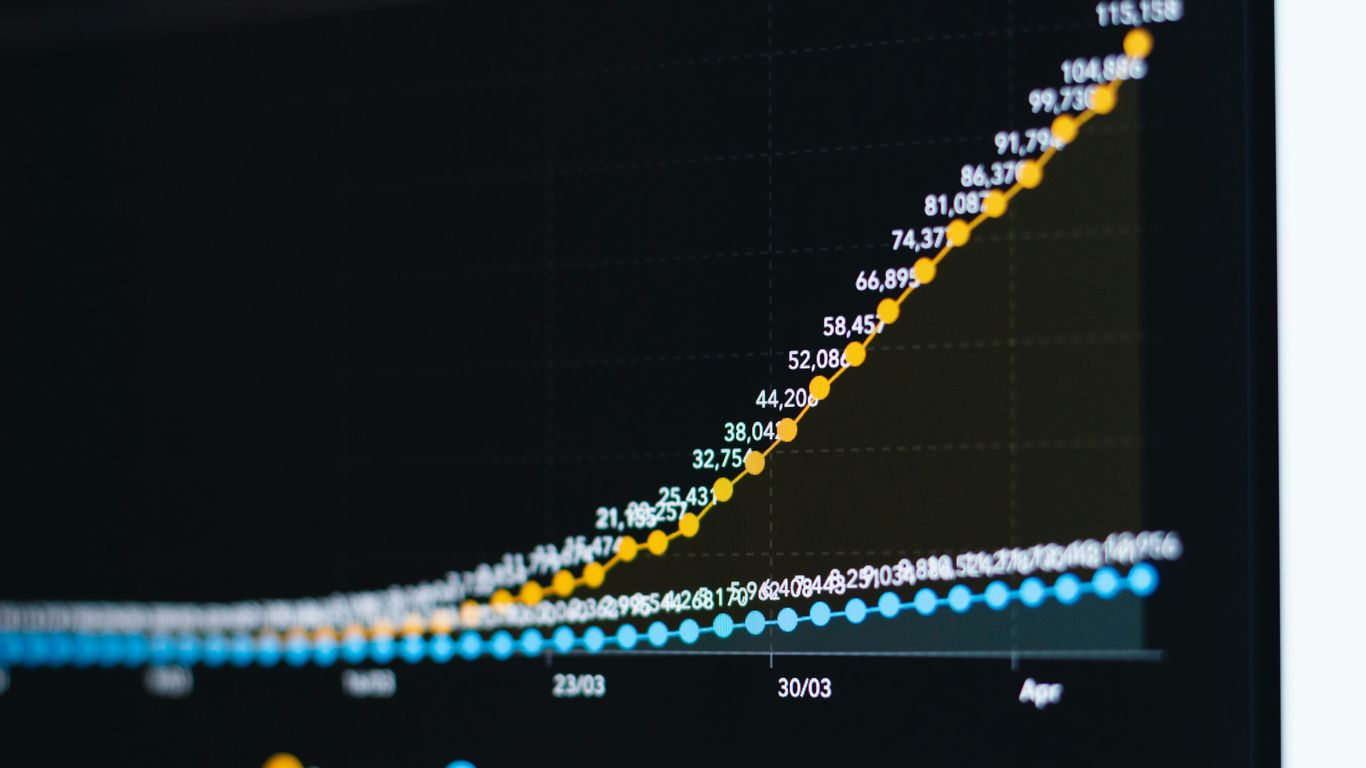
Real-Time Analytics for Financial Performance
It’s not just about automation; it’s also about knowing what’s happening with your money right now. Athenahealth gives you real-time stats on how your revenue is looking, where your claims are at, and your overall financial health. This kind of information helps you spot problems early, figure out when payments might be delayed, and fix billing issues before they get too big. It’s like having a crystal ball for your practice’s finances.
Cloud-Based Solutions for Accessibility and Efficiency
Being stuck in the office to access billing data is a thing of the past. Athenahealth’s cloud-based system means you can get to your financial information from pretty much anywhere. Plus, software updates happen automatically, and staying compliant with rules is easier. This approach cuts down on the need for expensive on-site computer systems and makes things more flexible, especially for practices that are growing. It’s estimated that about 78% of healthcare groups using cloud billing are seeing better operations and saving money.
The move from manual billing to digital systems has been a huge step forward for medical practices. It’s made claims more accurate, processing faster, and ultimately improved how practices get paid. Electronic transactions alone are estimated to save the US healthcare system billions each year in administrative costs. Athenahealth’s focus on cloud computing, real-time claim tracking, and automatic error detection helps practices reduce claim rejections and get paid quicker, making the whole revenue cycle run much smoother.
Key Developments in Athenahealth’s Offerings
New AI-Native Features in athenaOne
Athenahealth has been busy rolling out new features built right into their athenaOne platform, and a lot of it centers around artificial intelligence. The goal here is pretty straightforward: make life easier for medical practices and speed up how they get paid. They’re talking about cutting down on the paperwork and busywork that eats up so much time, potentially by more than half for some practices. This push towards AI-native tools is designed to help practices get their claims paid faster and improve their overall financial health.
Think of it like this: the system is learning from billions of claims and payer rules. This helps it automate tasks that used to require a person to do them manually. Features like automatic insurance selection, AI agents that can deal with payer portals, and smarter scheduling are all part of this. It’s all about making the process smoother and getting cleaner claims out the door the first time.
The company’s approach is to use its cloud-based, AI-native setup to quickly add new AI capabilities. This means they can innovate faster and really change how revenue cycle management works for their clients, setting them up for better financial results down the road.
Focus on Reducing Administrative Workload
One of the biggest headaches in running a medical practice is all the administrative stuff that piles up. Athenahealth seems to be really zeroing in on this. They’re not just talking about small tweaks; they’re aiming for a big reduction in the day-to-day tasks that take clinicians and staff away from patient care. This includes things like managing patient appointments, handling insurance paperwork, and following up on payments. By automating these kinds of jobs, they hope to free up a significant amount of time.
Here’s a look at some of the areas they’re targeting:
- Patient Scheduling: Making it easier to book and manage appointments, reducing no-shows.
- Billing and Claims: Automating claim submission, checking for errors, and following up on denials.
- Patient Communication: Streamlining how practices communicate with patients about appointments and bills.
- Data Entry: Reducing the need for manual input of patient and insurance information.
Accelerating Reimbursements and Improving Financial Outcomes
Getting paid quickly and accurately is obviously super important for any healthcare practice. Athenahealth’s recent developments are heavily focused on making this happen. They’re using their network and AI tools to speed up the reimbursement cycle. This means less waiting around for checks and fewer claims getting rejected, which can really impact a practice’s bottom line.
Here’s how they’re working on it:
- Claim Accuracy: AI helps catch errors before claims are sent, leading to fewer denials.
- Faster Follow-up: Automated systems can chase down unpaid claims more efficiently than manual processes.
- Real-time Financial Data: Cloud-based systems give practices a clearer, up-to-the-minute view of their financial performance.
- Predictive Analytics: Using data to identify potential payment issues before they become big problems.
It’s all about making the financial side of running a practice less of a struggle and more predictable. They’re aiming for near-perfect claim acceptance rates, which sounds pretty good, right?
Athenahealth’s Commitment to Customer Success
Value-Based Care Support
Athenahealth really gets that healthcare is changing, and they’re putting a lot of effort into helping practices get ready for value-based care. This means shifting from just doing more services to actually focusing on patient health outcomes and doing it efficiently. They provide tools and guidance to help practices track patient progress, manage chronic conditions better, and get paid for the quality of care they provide, not just the quantity of appointments. It’s about making sure practices can succeed financially while also improving how they care for people.
Customer Success Community Engagement
It’s not just about the software; it’s about the people using it. Athenahealth has built a pretty active online community where users can connect, share tips, and ask questions. This space is a big deal because it lets practices learn from each other and from Athenahealth’s own experts. With over 44,000 monthly active users, it’s a place where you can find answers and support, making sure you’re getting the most out of the platform. This network of users is a key part of their customer success strategy.
Cost and Value Proposition
When it comes to the money side of things, Athenahealth ties its success to yours. Their model often means they get paid when you get paid, which is a pretty clear sign they’re invested in your financial performance. They aim to provide a system that not only works well but also makes financial sense for practices, especially with the increasing focus on value-based care. They believe their integrated approach, combining technology and services, offers a strong return on investment by improving efficiency and revenue.
Here’s a quick look at some numbers that show their reach:
| Metric | Figure |
|---|---|
| Providers on the network | 160K+ |
| Patient records migrated | 158M+ |
| Monthly active community users | 44K+ |
The focus on customer success isn’t just a buzzword for Athenahealth. It’s built into how they operate, from their payment models to the resources they provide. They understand that for their platform to be truly effective, practices need ongoing support and a community to learn from. This approach helps practices adapt to the evolving healthcare landscape and achieve better results for both their patients and their bottom line.
Technological Advancements in Billing Efficiency
Remember the days of mountains of paperwork and endless phone calls to chase down payments? It feels like a lifetime ago, doesn’t it? Medical billing used to be a real headache, full of delays and mistakes that could really mess with a practice’s finances. But things have changed, big time. We’re talking about a shift from those slow, paper-based methods to slick digital workflows. This move to technology has seriously boosted how accurate and fast claims get processed. It’s not just about making things quicker; it’s about getting paid faster and keeping the practice running smoothly.
Evolution from Manual to Digital Billing
Back in the day, billing was a manual slog. You’d fill out forms, mail them off, and then wait. And wait. Errors were common, payments got delayed, and it took a ton of staff time just to keep things moving. Now, with digital systems, it’s a whole different ballgame. Electronic transactions alone are estimated to save the U.S. healthcare system billions each year in administrative costs. Computerized claims processing cuts down on denials and makes sure everyone’s following the rules.
Benefits of Integrating Technology in Billing
So, what’s the big deal with all this tech? For starters, accuracy gets a major upgrade. Think automated claim scrubbing that catches errors before they get sent out, or AI that helps make sure the right codes are used. This means fewer rejected claims and less back-and-forth. Plus, real-time eligibility checks mean you know if a patient is covered before they even leave the office. It also means faster payments because electronic remittance advice posts payments way quicker than manual methods. And let’s not forget administrative efficiency – automating tasks frees up your staff to do more important things than data entry.
Here’s a quick look at some key benefits:
- Fewer Errors: Automated checks catch mistakes early.
- Faster Payments: Electronic processes speed up reimbursement.
- Better Financials: Reduced denials and improved collection rates.
- More Staff Time: Automation handles repetitive tasks.
The move to digital billing isn’t just a trend; it’s a necessity for practices looking to stay financially healthy and operationally sound in today’s healthcare landscape. It allows providers to focus more on patient care and less on the administrative maze.
Addressing Implementation Challenges and Security
Of course, switching to new tech isn’t always a walk in the park. There can be hurdles. Training staff takes time and resources, and getting new systems to play nice with existing ones (like your EHR) can sometimes be tricky. There are also initial costs to consider. But here’s the thing: Athenahealth works to make this transition smoother. They often use cloud-based solutions, which means easier updates and remote access, cutting down on the need for expensive on-site hardware. And when it comes to security, protecting patient data is paramount. Think encryption, secure access controls, and regular compliance checks to keep everything safe and sound, meeting rules like HIPAA.
Wrapping It Up
So, what’s the takeaway from all this? Athenahealth is clearly pushing forward, especially with their focus on AI and making things work better for doctors and their staff. They’re talking about cutting down on paperwork and getting paid faster, which, let’s be honest, is a huge deal for any practice. With a big network already in place and new tools coming out, it seems like they’re trying to keep up with the fast pace of healthcare tech. It’s not always a smooth ride for everyone, as some users mention challenges, but the direction they’re heading seems to be all about making the day-to-day operations smoother and more efficient. We’ll have to keep an eye on how these changes play out for the practices using their systems.








