Hospitals are changing, and it’s all about putting the patient first. We’re seeing a lot of new ideas and tech pop up that aim to make hospital stays better, more comfortable, and more effective for everyone involved. From how rooms are designed to the tools doctors use, the focus is shifting. It’s about making healthcare work better for the people it serves, and that means listening to what patients and their families need and want. This article looks at some of the latest innovation in hospitals that are making this patient-centric approach a reality.
Key Takeaways
- Patient-centered care means putting individual health needs and goals at the heart of all medical decisions and making patients active partners in their treatment.
- New technologies are transforming hospital spaces, making them more comfortable and giving patients more control over their care, with trends towards smaller, specialized centers.
- Today’s patients are more informed and expect high-quality, accessible care, driving demand for user-friendly medical devices and personalized treatments.
- Hospitals are creating more welcoming, home-like environments and integrating family members as part of the care team to improve recovery and well-being.
- Digital tools and AI are helping to connect health data, improve communication, and tailor treatments, making healthcare more efficient and personalized.
Embracing Patient-Centricity in Healthcare
It’s a big shift, really, moving from a system where doctors and nurses were the sole decision-makers to one where the patient is truly at the center of everything. This isn’t just a buzzword; it’s about fundamentally changing how care is planned and delivered. Think of it as a partnership, where your needs and what you hope to achieve with your health are the main focus. It means looking beyond just the illness and considering how it affects your life – your emotions, your social connections, even your finances.
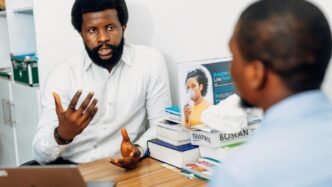
Defining Patient-Centered Care
At its core, patient-centered care means that every decision, every plan, and every quality check is driven by what the individual patient needs and wants for their health. It’s about treating people as partners in their own care. Providers aren’t just looking at symptoms; they’re considering the whole person. This approach aligns the entire healthcare system, from its mission and leadership down to daily operations, with the goal of putting the patient first. It’s about making sure the right care happens at the right time and in the right place, always with the patient’s preferences and values in mind.
Elements of Patient-Centered Care
So, what does this look like in practice? Several key elements stand out:
- Collaboration and Shared Decisions: Patients and their families are active participants in creating and managing care plans. This isn’t a top-down approach; it’s a team effort.
- Respect for Individuality: Care plans and treatments take into account a patient’s personal values, cultural background, and even their socioeconomic situation. What works for one person might not work for another.
- Open Information Sharing: Patients and their families receive clear, timely information so they can make informed choices about their health. No more feeling left in the dark.
- Comfort and Well-being: The focus is on both physical comfort and emotional support throughout the care journey.
- Family Integration: Family members are not just visitors; they are encouraged to be part of the care team, present during discussions and involved in decisions. Hospitals are even redesigning spaces to be more welcoming for families.
Benefits for Patients and Providers
This shift isn’t just good for patients; it benefits everyone involved. For patients, the primary gain is improved health outcomes tailored to their specific situation. But it goes further. Patients often report higher satisfaction with their care. For providers and the healthcare system, the advantages include better staff morale, a stronger reputation among the public, and more efficient resource use. When patients are engaged and satisfied, it creates a more positive and productive environment for everyone. For instance, wearable devices are becoming increasingly important tools for patients to track their own health data, contributing to better self-management and communication with their doctors. You can learn more about how these devices are changing lives at wearable technology.
Ultimately, patient-centered care is about recognizing that healthcare is most effective when it’s built around the person receiving it, not just the condition they have.
Technological Advancements Driving Innovation in Hospitals
It feels like every week there’s some new gadget or system promising to make hospitals run better and make patients happier. And honestly, a lot of it is pretty cool. We’re seeing technology change not just the machines we use, but how the whole place looks and feels.
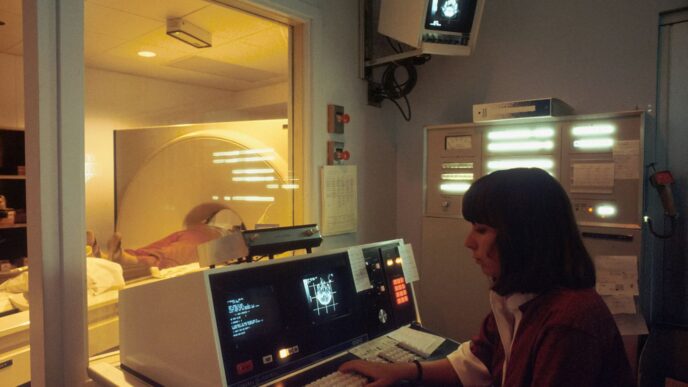
Revolutionizing Healthcare Spaces with Technology
Think about it: hospitals used to be pretty sterile, right? Now, places are being designed from the ground up with technology in mind. This isn’t just about having Wi-Fi everywhere, though that’s a start. It’s about creating environments that actually help people heal. For example, some new hospitals are built to easily add future tech, whatever that might be. At the same time, the pandemic got us thinking differently about where care happens. We’re seeing more smaller, specialized clinics and even mini-hospitals popping up. These places often focus on specific complex cases and are designed to be more efficient, partly thanks to smart tech integration. The goal is to make things better for everyone – patients, their families, and the staff. It’s about reducing how long you wait, giving you more control over your own care, and generally making the whole experience less stressful.
Improving Patient Comfort and Autonomy
Technology is also stepping in to give patients more say and make their stay more comfortable. Imagine being able to control your room’s lighting, temperature, or even order meals right from a tablet. That kind of control can make a big difference when you’re feeling vulnerable. It’s about shifting from a passive patient role to a more active one. This also ties into making spaces feel less institutional and more like a place where you can actually recover. Think about better ways to communicate with your care team, getting information when you need it, and having tools that help you manage your own health needs during your stay.
Wearable Devices and Remote Diagnostics
This is where things get really interesting for keeping an eye on health outside the hospital walls, but it’s also starting to show up inside. Wearable devices, like smartwatches that track heart rate or activity, can give doctors a constant stream of data. This means they can spot problems early, sometimes before you even feel sick. For remote diagnostics, think about telehealth appointments where a doctor can see and talk to you, or even use connected devices to check certain vital signs. Inside the hospital, these kinds of tools could mean less need for constant check-ins by nurses for basic readings, freeing them up for more critical tasks. It’s a way to keep a closer watch on patients without being intrusive, and it’s definitely changing how we think about monitoring health.
The Evolving Patient and Healthcare Consumerism

It feels like just yesterday we were passively accepting whatever the doctor said. Now? Not so much. Patients today are way more informed, and honestly, they expect a lot more. Think about it – we research everything else online, so why not our health? This shift means people are taking charge of their own well-being, wanting to be part of the decision-making process, and looking for care that fits their lives, not the other way around.
Increased Patient Independence and Engagement
People aren’t just showing up for appointments anymore; they’re actively participating. They want to understand their conditions, explore treatment options, and have a say in their care plan. This independence is fueled by readily available information and a desire for more control over personal health matters. It’s a good thing, really, as engaged patients tend to have better outcomes.
Demand for High-Quality, Accessible Care
Along with wanting to be involved, patients are also looking for care that’s not only good but also easy to get. This means convenience is key. Whether it’s telehealth options, flexible appointment times, or clear communication, people want healthcare that fits into their busy schedules. And let’s not forget the cost factor; everyone’s looking for value, wanting the best possible care without breaking the bank.
Patient-Centric Innovations in Medical Devices
This demand for better, more accessible care is pushing medical device companies to get creative. We’re seeing devices that are less invasive and more user-friendly. Remember those old, bulky machines? Many are being replaced by smaller, more portable versions that give patients more freedom. Even things like continuous glucose monitors are becoming less of a hassle, making it easier for people to manage chronic conditions at home. It’s all about making healthcare fit the patient, not forcing the patient to fit healthcare.
Transforming the Hospital Experience
Family Integration in the Care Team
Bringing families into the loop is a big deal now. It’s not just about having a visitor; it’s about making them part of the actual care plan. Think of it like this: when a kid is in the hospital, their parents know them best. They can spot subtle changes or understand what might be upsetting them. Hospitals are starting to see this and are creating ways for families to be more involved, like having a parent stay overnight or even helping with certain care tasks under supervision. It makes the patient feel more secure and can actually speed up recovery because they’re less stressed.
Home-Like Environments for Enhanced Recovery
Nobody really wants to be in a hospital. They’re often sterile and a bit impersonal. So, the trend is to make them feel more like home. This means softer lighting, less noise, and more comfortable furniture. Some places are even using calming colors or bringing in plants. For kids, this could mean themed rooms or play areas. The idea is that if a place feels less like a hospital and more like a comfortable space, people will feel more relaxed and heal better. It’s about creating an atmosphere that supports healing, not just treats illness.
Personalized Medicine and Tailored Therapies
We’re moving away from one-size-fits-all treatments. Now, doctors are looking at a person’s unique genetic makeup, lifestyle, and even their environment to figure out the best way to treat them. This means therapies are becoming more specific. For example, instead of a general chemotherapy drug, a patient might get a drug that’s specifically designed to target the particular type of cancer cells they have. This approach aims to be more effective and reduce side effects. It’s a complex process, but it’s all about making sure each patient gets the exact care they need, right when they need it.
Leveraging Digital Solutions for Enhanced Engagement
It’s pretty clear that digital tools are changing how hospitals work with patients. Think about it – we’re not just talking about booking appointments online anymore. We’re seeing a big shift towards patients being more involved in their own care, and technology is a huge part of that.
Breaking Down Data Silos with Digital Platforms
One of the biggest hurdles hospitals face is when information is scattered everywhere. Different departments might have different systems, and getting a clear picture of a patient’s history can be tough. Digital platforms are starting to fix this. By bringing patient data together in one place, like electronic health records (EHRs) that actually talk to each other, doctors and nurses can see the whole story. This means fewer mistakes and better decisions.
- Improved Care Coordination: When all patient information is accessible, care teams can work together more effectively.
- Reduced Redundancy: Patients don’t have to repeat their medical history over and over.
- Data-Driven Insights: Hospitals can analyze trends to spot areas for improvement.
Collaborative Engagement Through Digitalization
Remember when healthcare felt like a one-way street, with doctors telling patients what to do? That’s changing. Digital tools are making it a two-way conversation. Patients can access their own health records, track their progress, and even communicate with their care team through secure portals or apps. This kind of engagement helps patients feel more in control and more likely to stick with their treatment plans.
- Patient Portals: Secure online access to medical records, test results, and appointment scheduling.
- Telehealth Services: Virtual visits that offer convenience and accessibility.
- Health Tracking Apps: Tools for patients to monitor vital signs, medication adherence, and symptoms.
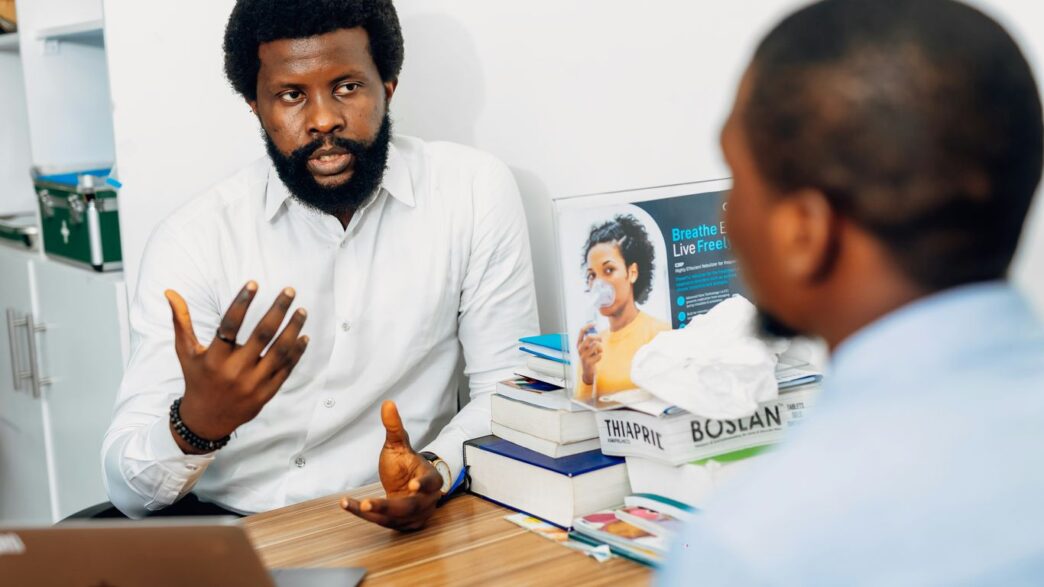
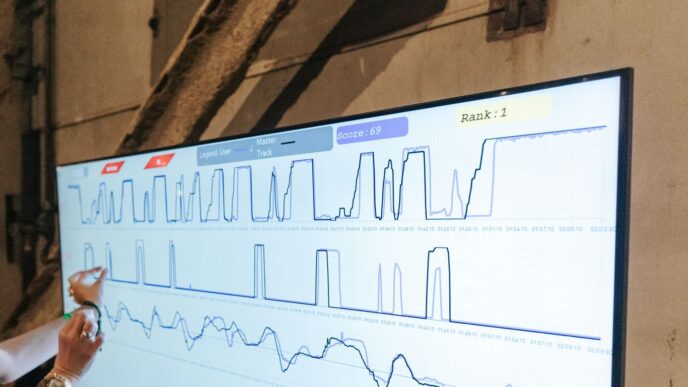
The Role of Artificial Intelligence in Healthcare
Artificial intelligence, or AI, is really starting to make waves. It’s not just about robots; it’s about smart systems that can help doctors diagnose illnesses faster, suggest personalized treatment plans, and even manage hospital operations more smoothly. AI can sift through massive amounts of data to find patterns that humans might miss, leading to more precise care. This technology has the potential to truly transform how we approach patient care. For example, AI can analyze medical images with incredible accuracy, helping to catch diseases earlier than ever before.
Strategies for Scaling Innovation in Hospitals
So, you’ve got a great idea, a pilot project that’s really showing promise in your hospital. Now what? Getting that innovation to spread beyond a single department or even a single hospital is where things get tricky. It’s not just about having a good concept; it’s about the nuts and bolts of making it happen on a larger scale.
Overcoming Barriers to Innovation Adoption
Let’s be real, hospitals are complex places. There are a lot of moving parts, and introducing something new can feel like trying to reroute a river. One of the biggest hurdles is often money. Budgets are usually department-specific, meaning if your innovation saves money in one area but costs a bit more in another, it’s hard to get buy-in. Think about it: if a new piece of equipment helps nurses save time, but the initial purchase price is high and the savings are spread across multiple departments, who’s going to champion that purchase?
- Fragmented budgets: Departments often operate with their own financial pots, making it tough to share costs or benefits of new initiatives. This can kill promising ideas before they even get off the ground.
- Data system limitations: If your hospital’s IT systems can’t talk to each other, tracking the impact of an innovation becomes a nightmare. You need good data to prove something works, and if you can’t get it, scaling is nearly impossible.
- Resistance to change: People get comfortable with how things are done. Even if a new way is better, getting everyone on board takes time, training, and a lot of communication.
The Importance of Stakeholder Collaboration
Nobody innovates in a vacuum, right? You need everyone rowing in the same direction. This means getting doctors, nurses, administrators, IT folks, and even finance departments talking to each other. When you have strong clinical leadership working hand-in-hand with executive support, and policies that actually make sense for new ideas, that’s when things start to move.
It’s also about building networks. Sharing what works (and what doesn’t) with other hospitals can prevent everyone from making the same mistakes. Imagine if a hospital in another city figured out a brilliant way to streamline patient admissions – sharing that knowledge could save countless hours and resources across the board. This is why aligning AI initiatives with both clinical and business objectives is so important for widespread adoption [886b].
Aligning Incentives for Better Patient Outcomes
Ultimately, people respond to incentives. If the system rewards sticking with the old ways, innovation will struggle. We need to look at how we pay for things. Are there ways to structure payments that encourage efficiency and new approaches? Maybe funding models that share the risk or reward successful outcomes could make a big difference. It’s about creating a system where trying new, better ways of doing things actually makes sense financially and operationally for everyone involved. This isn’t just about adopting new tech; it’s about rethinking how the whole system works to benefit patients.
Moving Forward: A Patient-First Future
So, we’ve talked a lot about how hospitals are changing, putting patients right at the center of everything. It’s not just about new gadgets or fancy buildings, though those play a part. It’s really about a shift in thinking, making sure patients and their families feel heard and are part of the care team. From how rooms are designed to how doctors talk to people, the goal is to make healthcare feel more human and less like a chore. It’s a big change, and it’s still unfolding, but the direction is clear: better care for everyone starts with focusing on the person receiving it.
Frequently Asked Questions
What does it mean for care to be patient-centered?
Patient-centered care means that doctors and hospitals focus on what *you* need and what you want to achieve with your health. You become a partner in your own care, and healthcare providers consider not just your physical health, but also how you’re feeling emotionally, mentally, and socially.
How do hospitals use technology to help patients?
Hospitals are using technology in many ways to make things better for patients. This includes designing spaces that feel more comfortable, like home, and using new tools that give patients more control over their health. Think of things like devices that help you track your health at home or easier ways to connect with your doctor.
Why are patients getting more involved in their healthcare decisions?
People today are more connected and informed about their health than ever before. They want to be active in making choices about their care, and they expect high-quality, easy-to-access medical help. This is why healthcare is becoming more focused on the patient’s needs and preferences.
How are hospitals changing to feel more welcoming?
Hospitals are trying to create environments that help people recover faster and feel more comfortable. This often means allowing family members to be more involved in care, creating rooms that feel more like home, and offering treatments that are specially made for each person’s unique needs.
What is the role of digital tools in improving patient care?
Digital tools, like online patient portals or health apps, help patients stay connected and informed. They can break down barriers to information, making it easier for patients and providers to work together. Artificial intelligence (AI) is also being used to help doctors make better decisions and offer more personalized treatments.
What are the biggest challenges in bringing new ideas to hospitals?
Bringing new ideas to hospitals can be tough. It often involves getting everyone on board, from doctors to administrators, and finding the money and resources to make changes. Sometimes, old ways of doing things or complicated rules can also get in the way of adopting new and better methods.