It’s a busy time in healthcare, with new ideas popping up all over the place. From how doctors treat patients to how companies develop new medicines, things are changing fast. We’re seeing a lot of focus on making things work better for people, using technology to help out. This article looks at some of the big trends and what they mean for everyone involved in health.
Key Takeaways
- MedCity News highlights how executives see healthcare changing, focusing on cost savings for employers and better ways to support doctors and patients.
- Personalized medicine and digital tools are becoming more important for managing long-term health issues and helping people stick to their treatment plans.
- The MedTech world is going digital, aiming for better teamwork and using things like AI and the Internet of Medical Things (IoMT) to improve patient care.
- Clinical trials are getting a makeover, with a push for simpler data, smarter ways to manage risks, and making it easier for patients to join in.
- Building trust in AI for healthcare means making sure it works well with doctors’ daily tasks and being open about how it makes decisions.
MedCity News: Innovations Shaping Healthcare’s Future

Healthcare is changing, and fast. We’re seeing a lot of new ideas pop up that are really shaking things up. It’s not just about new gadgets, but how we think about treating people, especially those with ongoing health issues. Companies are looking at ways to make care more personal, which makes a lot of sense when you think about it.
The big push is towards making healthcare work better for each individual person. This means looking at things like how we manage long-term illnesses, like diabetes or heart disease. Instead of a one-size-fits-all approach, the focus is shifting to treatments and support that are tailored to a person’s specific needs and lifestyle. It’s about giving people the tools and information they need to manage their own health more effectively.
We’re also seeing a lot of digital tools being developed, especially for people taking medications. These apps and platforms are designed to help patients remember to take their medicine, understand how it works, and generally stick to their treatment plans. For drug companies, this is a way to support patients beyond just handing them a prescription. It’s about building a relationship and helping them get the best results from their treatment.
Here’s a quick look at some of the key areas driving these changes:
- Personalized Care: Moving away from generic treatments to plans designed for the individual.
- Chronic Condition Management: Developing better ways to support people living with long-term illnesses.
- Digital Support for Pharma: Creating apps and tools to help patients adhere to their medication and treatment plans.
The Digital Transformation of MedTech
The medical technology sector is really changing, and it’s all thanks to digital tools. We’re seeing a big shift towards making healthcare more connected and focused on the person receiving care. It’s not just about new gadgets anymore; it’s about how these technologies work together to improve things for everyone involved.
Improving Collaboration for a Patient-Centric Ecosystem
Getting everyone on the same page is a big deal in healthcare. MedTech companies are now building platforms that help doctors, hospitals, and even patients share information more easily. This means better coordination, especially for people with ongoing health issues. Think about it: if your doctor, specialist, and physical therapist can all see your latest test results instantly, it makes managing your health so much smoother. This move towards an open system is key to putting the patient at the center of their own care.
The Role of AI and Cloud in MedTech Advancements
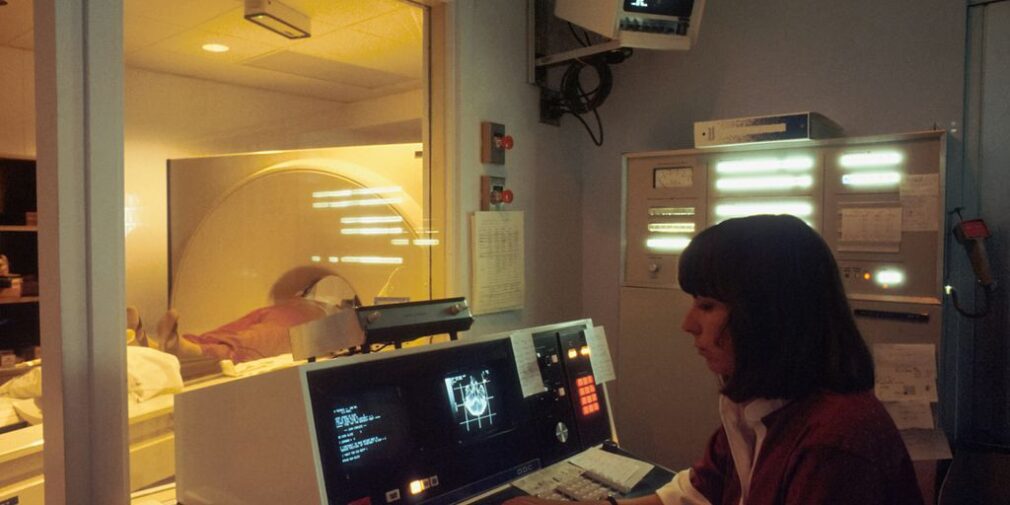
Artificial intelligence (AI) and cloud computing are like the engines driving this digital transformation. AI can look at medical images, like X-rays or scans, and spot things that might be missed by the human eye, helping doctors catch diseases earlier. The cloud, on the other hand, allows for massive amounts of patient data to be stored and accessed securely, making it possible for remote monitoring and personalized treatment plans. It’s pretty amazing how much data these devices can collect and how AI can make sense of it all.
Enhancing Patient Care Through IoMT and Digital Platforms
The Internet of Medical Things (IoMT) is a big part of this. It’s basically a network of connected medical devices – like smartwatches that track your heart rate or glucose monitors that send readings directly to your doctor. These devices allow for continuous patient monitoring from home, which is a game-changer, especially for managing chronic conditions. Digital platforms are also popping up that use things like virtual reality for therapy or provide apps to help patients stick to their medication schedules. These digital tools are making healthcare more accessible and tailored to individual needs.
Advancements in Medical Devices and AI
It’s pretty wild how fast things are changing in medical devices and AI, right? Just last year, we saw a huge jump in FDA approvals for new medical gadgets, and a good chunk of those were powered by AI. This really shows that digital ways of taking care of people are becoming the norm, aiming to get better results for patients. For example, a new AI tool that helps doctors catch early signs of heart problems got the green light recently. It feels like the focus on improving care quality is really picking up speed.
FDA Approvals Highlight Digital Care Delivery
Last year was a big one for MedTech, with lots of new tech coming out. The number of FDA approvals for novel medical devices hit an all-time high. Many of these were AI-driven. This is a clear sign that digital care is gaining traction, with the goal of improving patient outcomes. Think about it: AI tools are now helping doctors spot early signs of conditions like heart failure, which is a big step forward in making care better.
AI Tools for Early Disease Detection
AI is really changing the game when it comes to finding diseases early. Imagine AI systems looking at images from colonoscopies in milliseconds, flagging anything that looks suspicious. These systems can sort through massive amounts of data to help doctors make better decisions and catch things like colorectal cancer much sooner. It’s not just about imaging, though. AI algorithms can also look at your medical history, your genes, where you live, and your lifestyle choices – all the stuff that devices collect – to suggest treatments, diets, and exercises that are just right for you. It’s about making care more personal.
Personalization and Digital Transformation in MedTech
MedTech companies need to keep up with these changes to stay competitive. Being an early adopter of new tech can give you an edge. Three main areas are really shaping the industry right now: the Internet of Medical Things (IoMT) for connected care, AI for smarter medical imaging and managing long-term health issues, and digital platforms that make care more accessible. For instance, many places are using smart devices with sensors that send patient data in real-time to AI-powered apps for remote monitoring. This is how connected medical devices are helping manage chronic conditions. The goal is to make care faster, easier to use, more inclusive, and safer, all while keeping costs down.
Streamlining Clinical Trials with Pragmatic Innovation
Clinical trials are getting pretty complicated, aren’t they? It feels like every new study needs more data, more checks, and more people involved. But there’s a push to make things simpler, to use what they’re calling ‘pragmatic innovation.’ Basically, it’s about being smart and flexible, ditching old ways that don’t work anymore, but without messing up the quality of the research. It’s a big shift, and it touches everything from how data is handled to how patients are included.
Simplifying and Standardizing Data in Clinical Research
Lots of people working with clinical data, even when they’re miles apart, are talking about the same thing: making data simpler and more uniform. This isn’t just a nice-to-have; it’s becoming necessary because the whole research landscape is so much more complex now. The FDA even put out some advice encouraging these more practical trial designs. Think about it like this: if a trial is set up to be more like what doctors and patients do every day, more people can actually join and contribute. It makes sense, right? Instead of trying to put every single piece of data into one giant system, which has been tough, the idea is to focus on the data that really matters for study design and analysis. This way, teams can work together better and get things done faster, from building the study to locking the data.
Risk-Based Quality Management in Clinical Trials
For a while now, regulators have been suggesting a ‘risk-based’ way of managing quality in trials. Still, many places stick to older methods that involve checking everything thoroughly. But leaders in the field see the value in focusing on risks. They’re starting to use better tools and train their data managers to move from just checking data to actually understanding it like scientists. Imagine a system where research staff can see what needs checking without downloading big reports or messing with spreadsheets. This could cut down on a lot of work and site visits. It’s about being proactive, spotting potential problems early using past data, and having plans in place to deal with them. This approach can lead to better data, more efficient use of resources, and getting new treatments to people faster.
Enhancing Patient Participation in Clinical Research
It’s kind of surprising, but only a small percentage of doctors and patients in the U.S. actually take part in clinical trials. This low number means that most studies miss their enrollment targets, causing costly delays. The focus is shifting from just where trials happen to how the whole experience is for everyone involved – patients, research sites, and the teams managing the data. The goal is ‘patient optionality,’ meaning patients can choose how they participate, whether that’s at home, a clinic, or a research site. This makes it easier for them and helps research move along efficiently. Companies are also looking at how many devices and tools they ask patients to use, trying not to overwhelm them. Sometimes, they’re even asking for less data during the trial itself, starting right from the initial study design. It’s all about making the patient experience better and gathering the information that truly counts.
IoMT and AI: Allies for Better Healthcare
The way we approach patient care is really changing, and a lot of that has to do with the Internet of Medical Things (IoMT) and artificial intelligence (AI). These aren’t just buzzwords; they’re becoming actual tools that help doctors and nurses do their jobs better and, more importantly, help patients get the care they need, often without even leaving their homes.
Remote Patient Monitoring with Connected Medical Devices
Think about it: instead of needing to go to the doctor’s office for every check-up, especially if you have a long-term health issue, you can now have devices at home that keep an eye on things. Wearable sensors, smart blood pressure cuffs, glucose monitors – these are all part of the IoMT. They collect data and send it securely to your healthcare team. This means doctors can see what’s happening with your health in real-time. If something looks off, they can step in sooner rather than later. It’s a big deal for managing conditions like heart disease or diabetes, and it really cuts down on unnecessary trips to the clinic. It’s like having a constant, gentle check-in from your medical providers. This kind of setup is really changing how we think about continuous health monitoring.
AI’s Role in Medical Imaging and Chronic Disease Management
AI is also making huge strides, especially when it comes to looking at medical images and managing ongoing health problems. For example, AI can be trained to look at scans, like X-rays or MRIs, and spot things that might be hard for the human eye to catch, or at least catch them much faster. This can lead to earlier diagnoses for serious conditions. When it comes to chronic diseases, AI can sift through mountains of patient data – things like medical history, genetic information, and even lifestyle habits – to help create more personalized treatment plans. It can suggest specific medications, diet changes, or exercise routines that are best suited for an individual. It’s about using data to make care more precise.
Personalized Treatment Through AI-Driven Data Analysis
So, how does this all come together for personalized treatment? Well, the data collected by IoMT devices, combined with other patient information, feeds into AI algorithms. These algorithms can then identify patterns and predict how a patient might respond to different treatments. It’s not a one-size-fits-all approach anymore. Instead, treatments are tailored to your specific biological makeup and lifestyle. This can mean better results and fewer side effects. The goal is to move towards care that’s not just reactive but also proactive and perfectly suited to each person. It’s a complex process, but the potential for improving patient outcomes is pretty significant.
Patient-Centricity in Clinical Trial Design
Getting people to sign up for clinical trials has always been a bit of a challenge. We’re talking about a tiny fraction of doctors and patients actually participating in studies for new treatments. This low number means a lot of studies miss their enrollment targets, which causes delays and costs a ton of money. The whole idea of decentralized clinical trials (DCTs) got people talking about where trials happen, but maybe not enough about the actual experience for the patients and everyone else involved. The industry is changing, though. Instead of just focusing on location, leaders are starting to think about giving patients more choices in how they take part. This means patients can decide if they want to participate from home, a clinic, or a research site. It’s about making research happen efficiently.
Sponsors are starting to look at the whole picture of a trial. They want to make sure patients aren’t overloaded with too many devices or apps. Having clear rules about using your own devices, like a phone or tablet, can make things easier for patients while still keeping the data safe and accurate. It’s also important to ask patients for less data when designing the study from the start. This means thinking about what actually benefits the patient before adding new things like electronic consent forms. Using surveys to understand how patients feel during a trial can help find ways to make it better.
Here are some key areas to focus on:
- Patient Optionality: Giving participants choices in how they engage with the trial, whether it’s through remote monitoring or in-person visits.
- Reducing Data Burden: Streamlining data collection to ask only for what’s truly necessary, making the process less demanding for participants.
- User-Friendly Technology: Implementing tools and platforms that are intuitive and easy to use, fitting into patients’ daily lives without causing undue stress.
Making patient optionality a reality is key to improving trial participation. It’s about designing studies that fit around people’s lives, not the other way around. This shift can help speed up research and bring new therapies to those who need them faster. For example, the new iPager from obsev aims to simplify communication, which could be a small step in making trial interactions smoother simplify communication.
Building Trust and Usability in Healthcare AI
It’s not enough to just have smart AI tools in healthcare. People actually have to be able to use them, and more importantly, trust them. Think about it: if a doctor can’t figure out how to use a new AI system, or if it gives advice that seems off, they’re not going to rely on it. That’s where building trust and making things usable comes in.
The real goal is to make AI feel like a helpful assistant, not a confusing black box.
So, how do we get there? It starts with how these tools are designed. They need to fit into how doctors and nurses already work. If a system requires a whole new set of steps or is hard to understand, adoption will be slow. We need AI that gives clear feedback and works with a clinician’s own judgment.
Here are a few things that matter:
- Clear Workflows: AI should slot into existing processes without causing major disruptions. Imagine an AI that helps flag potential issues in scans, but does it right there on the screen the radiologist is already using.
- Explainability: Doctors need to know why the AI is suggesting something. If an AI recommends a treatment, it should be able to show the data or reasoning behind that choice. This helps build confidence.
- Control: Clinicians must be able to override the AI when their experience tells them to. AI should support, not dictate, decisions.
Then there’s the whole idea of vertical integration. This is when different parts of a tech system, like the AI model, the user interface, and how data flows, are all controlled by one company. It can make things simpler for the user, sure. But in healthcare, this can also create problems. If one company controls everything, it might limit choices for others or create a closed system that’s hard for new ideas to get into. We need to be careful about creating "walled gardens" that stifle innovation and limit access for patients and providers.
To keep things fair and open, we need common standards and clear rules. This way, everyone can access and use these AI tools without being locked into one provider.
Finally, we have to think about the ethical side. AI in healthcare has huge potential, but it also carries risks. Bias in the data can lead to unfair outcomes for certain groups. Inaccuracy can cause harm. We need systems that can:
- Detect and reduce bias.
- Track how decisions are made (traceability).
- Explain their reasoning (explainability).
- Get consent from patients.
- Have plans for when things go wrong.
Building this ethical foundation isn’t just about following rules; it’s about making sure AI is a reliable and fair tool for everyone. It’s the bedrock for AI to be useful in healthcare for the long haul.
Looking Ahead
So, what does all this mean for the future of healthcare? It’s clear that technology is changing things fast. From making care more personal with things like AI and connected devices, to simplifying how we run medical studies, the goal is always to help people get better care, more easily. We saw how companies are using new tools to help employers manage costs, make doctors’ jobs less of a hassle, and get care to more people. It’s a lot to take in, but the main idea is that by working together and using these new ideas, we can build a healthcare system that’s better for everyone involved.














