Medtech cybersecurity is a big deal these days. With more medical devices getting connected, the risks are growing fast. It’s not just about keeping data safe anymore—patient safety and business survival are on the line. Hospitals, device makers, and even regulators are all scrambling to keep up. In this article, we’ll look at the latest threats, how to build safer devices, what rules you need to follow, and why working together matters. Let’s break down what’s happening and what everyone needs to do to keep healthcare safe in a connected world.
Key Takeaways
- Cybersecurity problems can delay up to 70% of new medical device approvals, making it a business and safety issue.
- Building security into devices from the start is now expected, not optional, especially as more devices connect to networks.
- Healthcare environments have unique risks, including older equipment and complicated data flows, which make them harder to protect.
- Staying on top of global rules—like those from the FDA and other agencies—is necessary for getting products to market and keeping patients safe.
- Teamwork across the industry, including sharing information and training, is key to staying ahead of new threats in medtech cybersecurity.
Emerging Threats and Vulnerabilities in MedTech Cybersecurity
Proliferation of Connected Medical Devices
If you look around modern hospitals, it’s like every device wants a Wi-Fi password—blood pressure monitors, infusion pumps, even digital thermometers. This trend means more entry points for hackers.
- Rapid growth in connected device deployments has opened new attack paths.
- Devices now often rely on wireless communication and cloud data transfer, increasing exposure.
- Many run on outdated or unsupported software, sometimes for years longer than a laptop or smartphone.
| Category | Estimated Devices in Use (2025) | Common Risks |
|---|---|---|
| Hospital Equipment | 400,000+ | Unpatched software, data leaks |
| Implantable Devices | 10 million+ | Wireless hijacking, replay |
| Home Health Devices | 150 million+ | Weak authentication, eavesdrop |
Every device added to a network is like another door that could potentially be left wide open. For medical devices, these open doors can impact real people, not just data or money.
Unique Risks in Healthcare Environments
Healthcare isn’t like other industries. There’s a mix of old and new equipment—and patient needs matter more than tech upgrades.
- Hospitals typically operate with a blend of legacy and modern medical devices.
- Maintenance windows are few because devices are needed almost constantly.
- Some staff may lack security training, making them more likely to fall for phishing or to ignore software update reminders.
Specific challenges:
- Patient safety comes first, which sometimes slows or complicates security updates.
- A single breach can expose a huge amount of personal health information.
- Healthcare networks are busy places, hard to monitor 24/7 with limited IT resources.
Impacts of Cyber Attacks on Patient Safety
This isn’t just about annoying pop-up ads or spam emails. When a medical device gets hacked, it can mess with care in real-time.
- Treatment delays if systems go down during a cyberattack.
- Altered readings from a compromised device can lead to wrong diagnoses or medication doses.
- Ransomware can freeze hospital operations, stopping surgeries or the use of life-support equipment.
These are not just tech problems—they become health emergencies fast. Protecting connected devices isn’t an option. It’s about keeping patients safe every single day.
Building Secure-by-Design Architectures for Medical Devices
Integrating Security into Product Development
Working security into a medical device’s life from day one is no longer just a good idea—it’s a must. Product teams should stop seeing cybersecurity as an add-on at the end. Instead, each phase, from requirements to deployment, should take possible threats, data privacy, and communication security seriously.
For every product release, threat modeling and regular code reviews can uncover bugs before they hurt patients or clinics. There are a few practical things to do:
- Map out all the connections—devices, users, networks—that will interact with the product.
- Set up layered defenses (like authentication, data encryption, and access controls).
- Regularly test the software for known flaws, like buffer overflows or poor configurations.
- Document security measures clearly for future updates and audits.
| Security Activity | When in Lifecycle | Example |
|---|---|---|
| Threat Modeling | Design | Attack trees, DFDs |
| Secure Coding Practices | Development | Input validation |
| Penetration Testing | Pre-market, Post-release | Network scans |
| Patch Management | Maintenance | Timely updates |
It’s all about making security just another part of building a usable and safe medical device—not an afterthought.
Zero-Trust Principles in Device Design
The old idea that anything inside a hospital’s network is safe doesn’t stand up anymore. Connected medical tools can be hacked anywhere along the line. That’s why more teams now use zero-trust.
Zero-trust means:
- Never automatically trust connections—always check the identity first.
- Authentications are strict and renewed often.
- Least-privilege rules: Users and apps only get exactly what they need, nothing else.
- Strong logging: Everything gets tracked for quick spotting of weird behavior.
It’s a mindset shift. Teams have to consider every single connection as suspicious until proven safe, just like cybercrime in other fields major security threats do to organizations.
Balancing Innovation and Safety
Medical devices are getting smarter and more connected, which is great for patient care but brings risk. The real challenge? Not letting security fears hold back fresh ideas or user-friendly features.
You can thread the needle with these habits:
- Open talks between clinical users, IT, and engineers—everyone shares what they need and what could go wrong.
- Prioritize risks: Focus first on changes that can really harm patients or leak data, before chasing optional features.
- Learn from real use: Keep shipping security updates and fixing gaps based on feedback instead of waiting for the next big redesign.
Balancing safety, speed, and real medical needs is hard work, but actually talking often—with the right people—makes it possible.
Navigating Global Regulatory Requirements in MedTech Cybersecurity
Staying on the right side of international rules is a real challenge for anyone working with medical technology. Companies in this space know that meeting global security standards isn’t just a box to tick—it directly impacts patient safety and business operations. Cybersecurity is now seen as a necessary piece of the puzzle for bringing new medical devices to market, not just an extra feature. Let’s break down what this looks like in practice.
FDA and International Compliance Standards
Medical device makers face a landscape of diverse and sometimes overlapping rules:
- The US Food and Drug Administration (FDA) expects security controls to be included in pre-market submissions and throughout a device’s lifecycle.
- Europe’s MDR and international standards like IEC 62304 and IEC 81001-5-1 also set specific expectations around cybersecurity management.
- The UK, Canada, and Australia each have their own guidance and approval processes—none identical.
Here’s a quick comparison:
| Region/Country | Key Standard/Guidance | Requires Security Plan? | Software Patch Rules |
|---|---|---|---|
| USA | FDA Pre-market Guidance | Yes | Update plan required |
| Europe (EU MDR) | IEC 62304, MDR | Yes | Requires update capabilities |
| Australia | TGA Guidance | Yes | Testing in live environment |
| UK | UKCA, MHRA | Yes | Patch impact review needed |
Getting a device certified in one country doesn’t mean it’ll automatically pass in another.
Aligning Security With Product Submissions
Security requirements start at step one. Here’s what most regulators look for during submission:
- Documented threat modeling and risk management plans
- Evidence of secure software and hardware development
- Policies for patching and managing vulnerabilities fast
Each submission asks for a slightly different format, but they all want proof you thought about security from the start. Skimp on robust documentation or leave gaps, and delays are almost certain.
Addressing Audit and Approval Delays
MedTech companies are seeing longer wait times due to cybersecurity hold-ups. In fact, more than half of new device submissions get flagged for missing or weak security details. That means:
- More back-and-forth with regulators
- Additional rounds of testing or documentation
- Last-minute design changes to address audit questions
Getting a product approved often feels like a marathon. Even a small documentation lapse can turn a big launch into a waiting game. Planning ahead for these requirements is the best way to avoid surprises.
When regulations change—as they often do—manufacturers need a plan to keep their devices up-to-date and compliant, even after release. That’s more patch testing, more paperwork, and sometimes, tough calls about when to sunset older models.
To sum it up, meeting global regulatory requirements takes time, attention to detail, and a process that puts security at the forefront from day one. It’s tough, but skipping steps here usually costs more in the end.
Operational Challenges in Safeguarding MedTech Ecosystems
Securing medical device systems isn’t a straightforward task. There are trade-offs everywhere—between performance, legacy compatibility, patient safety, and innovation. The push toward interconnected medical devices has opened up a whole new set of operational challenges that weren’t even on the radar a decade ago. Let’s get into some of the key sticking points.
Device Interoperability and Data Flow Risks
If you walk through any hospital, you’ll see devices from a dozen manufacturers, all needing to talk to each other. They push data between systems in real-time: imaging machines, infusion pumps, monitoring devices, and electronic health records are all part of the mix. When devices aren’t designed to coordinate securely, massive security gaps can emerge.
Main hurdles here:
- Mismatched security standards between devices
- Unprotected data as it moves (especially in legacy systems)
- Authentication difficulties when plugging in new devices
- The risk of data leaks when poorly handled integrations expose sensitive information
| Challenge | Impact | Potential Solution |
|---|---|---|
| Security standard gaps | Easy entry point for cyberattacks | Secure integration layers |
| Unencrypted data flow | Patient info exposed during transfer | End-to-end encryption |
| Device authentication | Unauthorized devices join the network | Robust device onboarding |
Smooth connectivity can make hospitals more efficient, but if the basics of authentication and encryption aren’t there, every new device is a new risk.
Monitoring and Incident Response
You can’t protect what you can’t see. In MedTech environments, device monitoring is tough for a few reasons:
- Unpredictable device behavior can lead to noisy alerts and false positives
- Many devices lack logging capabilities, making forensic work after an incident almost impossible
- Security teams have a tough time simulating attacks and preparing for real breaches due to hardware constraints
- There’s no unified dashboard—security info is scattered across device vendors and hospital IT
Some practical steps hospitals and manufacturers have started to take:
- Deploy network monitoring tools tailored for medical networks, not just IT
- Push firmware and software vendors to build in log and alerting features
- Encourage information sharing so lessons from one incident can help others
Legacy Device and Network Management
Let’s be honest—medical environments run on old tech. A big percentage of active devices are running out-of-support operating systems. These systems can’t always run modern security software, and patching them might not even be possible without breaking them.
Common legacy hurdles:
- Proprietary systems: Standard tools don’t always work out-of-the-box
- Unpatchable flaws: Sometimes, there’s simply no fix
- Complex dependencies: One weak old device might connect to multiple networks
A few things that help keep old devices safer:
- Segmenting these devices from critical hospital networks
- Monitoring unusual communication patterns as a sign of compromise
- Keeping careful records so known issues don’t slip through the cracks
Most hospitals will never be able to replace all their outdated tech overnight, so practical risk management here is more about smart isolation and layered monitoring than sweeping upgrades.
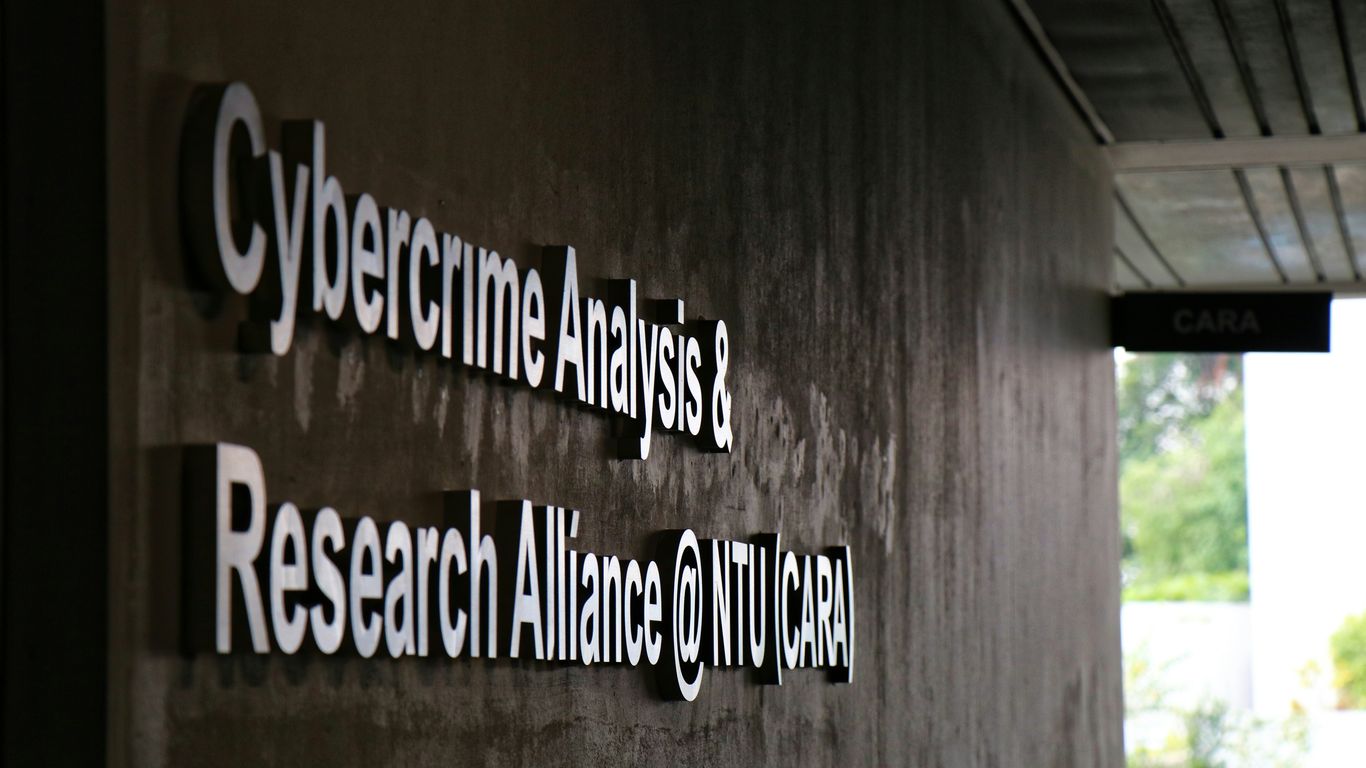
Collaborative Strategies for Advancing MedTech Cybersecurity
Keeping up with cybersecurity in medical technology takes more than just strong software. It’s about people, too. From device makers to hospital staff, everyone needs to work together so that both patient safety and business growth are protected. Let’s break down how this can work in practice.
Cross-Disciplinary Partnerships and Training
Cybersecurity for medical devices isn’t just a job for the IT department. Input from biomedical engineers, clinical staff, and compliance teams shapes safer solutions. Here’s how groups can get on the same page:
- Hold regular mixed-team simulation exercises. Bring together engineers, clinicians, and IT to see how they’d respond to real threats.
- Make cybersecurity skills part of staff onboarding and annual refreshers, not a one-off activity.
- Encourage open feedback loops between technical and non-technical staff to spot process gaps before hackers do.
A training culture that favors asking questions over hiding mistakes can turn potential disaster into a learning moment, and that kind of attitude keeps systems safer in the long run.
Industry Collaboration and Knowledge Sharing
Medical device manufacturers are realizing that sharing threat intelligence isn’t about giving away secrets—it’s about staying prepared. Competitive advantage shouldn’t come at the cost of widespread vulnerability. Here are three ways companies share the load:
- Participate in joint cybersecurity working groups or forums (like ISACs for healthcare).
- Use anonymized reporting tools so problems are flagged without fear of reputational loss.
- Adopt industry-wide checklists and standards for common device types, so no one is starting from scratch.
Here’s a simple table summarizing benefits seen by organizations that join collaborative security communities:
| Collaboration Activity | % Organizations Noting Improved Security | Example Benefit |
|---|---|---|
| Regular threat intelligence | 78% | Faster patch cycles |
| Co-developed response plans | 66% | Lower recovery time after incident |
| Standards adoption | 62% | Easier regulatory submissions |
You can read more about how collective innovation is impacting the broader technology landscape in key technology trends.
Engaging Healthcare Providers in Cyber Defense
Hospitals and clinics use these devices day in and day out. Keeping them in the loop can catch problems before they grow. Here are some core strategies:
- Build easy incident-reporting systems for front-line staff.
- Host joint post-incident reviews to find process fixes, not just patch software.
- Offer simple, jargon-free guidance tailored for clinicians, not tech experts.
The most effective cybersecurity practices in MedTech involve active, ongoing cooperation at every stage—from the drawing board to the hospital floor.
When organizations work together instead of in isolation, not only are patients safer, but the industry adapts faster to new security challenges. This approach isn’t just good for compliance—it’s a smart way to build trust and deliver care safely in a connected world.
Proactive Risk Management in a Connected Healthcare World
With healthcare networks more connected than ever, risk management goes from a checklist item to an everyday requirement. It’s not just about fixing something after it goes wrong.
Staying on top of new risks means gathering information from different sources and then actually doing something with it. Constantly scanning for new threats is mandatory, not optional. Here’s how to make it manageable:
- Use automated tools to conduct regular device and network scans.
- Subscribe to threat intelligence feeds that issue alerts specific to medical technology.
- Organize frequent tabletop exercises (once or twice a year) where real-world cyber attack scenarios test your team’s response.
Every hospital or clinic is different, but treating cybersecurity like one more compliance box only gets you in trouble when the inevitable incident happens.
Being proactive means monitoring systems 24/7, with alerts set up for anything unusual. Don’t wait for a researcher to warn you; know before an attacker does.
| Monitoring Method | What It Catches | How Often |
|---|---|---|
| Log Analysis | Suspicious activity | Daily |
| Network Monitoring | Unusual data transfers | Real-time |
| Device Status | Unauthorized changes | Hourly |
Consider these steps:
- Deploy sensors on major segments of your medical network.
- Make use of dashboards that filter the important alerts from the noise.
- Ensure alerts go to both IT and clinical engineering teams so nothing gets missed.
The reality is, attacks will happen. How you react is what makes the difference for patient safety and ongoing operations.
- Draft and update an incident response plan that covers who does what and when.
- Schedule regular hands-on drills for technical teams and non-technical staff alike.
- Maintain a list of all connected medical devices, updating it as new ones appear.
- Invest in data backup systems that recover patient information quickly after a breach.
Preparation means fewer surprises. Even a two-hour drill can reveal gaps that policy documents won’t.
Getting ahead of MedTech security risks takes patience and routine attention. But hospitals that do the work early avoid chaos and keep patient safety as their top focus.
Future Trends Shaping MedTech Cybersecurity
The way medical technology connects people and data is changing quickly, and so are the threats that come with it. Here’s what stands out on the horizon for MedTech cybersecurity, as we look toward tomorrow’s challenges and solutions.
Evolving Attack Vectors and New Technologies
Hackers aren’t standing still. As medical devices become smarter and more connected—to hospital networks, cloud platforms, and even each other—attack strategies are getting more creative. Tomorrow’s cyberattacks will target both the flow of information and the devices’ core functions, making regular software patches and hardware upgrades even more important.
- Attackers may exploit not only data exchanges, but also the inner workings of sensors and AI-driven diagnostics.
- Devices often share resources on large hospital networks, so a vulnerability in one tool could mean a risk for the whole system.
- Emerging technologies like 5G and IoT hubs, while making real-time care easier, also add fresh openings for cybercriminals.
It’s not just about locking the front door anymore. Every corner of the connected healthcare system has to be watched, or threats will slip in unnoticed.
The Role of Artificial Intelligence in Security
AI is already being trained to spot weird activity on medical networks. In the next few years, expect smart algorithms that:
- Monitor traffic between devices to catch threats much faster than humans can.
- Predict where attacks might happen, based on risk patterns.
- Automate responses—blocking suspicious access or isolating infected machines the moment something is off.
Here’s a quick look at how AI in MedTech security compares to traditional methods:
| Feature | Traditional Security | AI-Driven Security |
|---|---|---|
| Threat Detection Speed | Minutes to hours | Seconds to minutes |
| Human Intervention | Frequent | Minimal |
| False Positives | Higher | Lower |
| Adaptability | Slower | Rapid |
Anticipating Regulatory Evolution
Regulations are catching up with the technology, but it’s a slow process. In the coming years, medical device makers will likely see:
- New rules requiring proof of cybersecurity controls before devices hit the market.
- More frequent updates to security standards, both in the U.S. and around the world.
- Hospitals asking for detailed security documentation up front, not later on.
Some steps companies may need to follow soon:
- Submit cybersecurity plans as part of every regulatory filing.
- Show evidence of regular vulnerability assessments and penetration testing.
- Respond quickly to new guidance—delays may block approvals or sales.
The takeaway? If you wait for new laws to tell you what to do, you’ll always be scrambling to catch up with cyber risks that move a lot faster than the legal system.
Conclusion
Wrapping things up, it’s clear that cybersecurity in MedTech isn’t just a technical box to check anymore. It’s become a real part of keeping patients safe and making sure new devices actually make it to market. With more devices talking to each other and sharing data, the risks just keep growing. The old ways of patching things up after the fact don’t cut it. Teams need to think about security from the very start, not as an afterthought. Regulations are getting tougher, and the cost of ignoring these issues can be huge—both for business and for patient care. The good news is, there are more resources and better tools out there than ever before. By working together and staying alert, the MedTech community can keep pushing innovation forward without putting safety on the back burner. It’s a challenge, but it’s one we can meet if we keep security front and center.