Artificial intelligence is changing a lot of things, and healthcare is definitely one of them. Specifically, ai medical diagnosis tool systems are popping up everywhere, making it easier for doctors and nurses to figure out what’s wrong with people. These systems can look at tons of information really fast, way faster than a person could. It’s pretty amazing how they can spot things that might be missed otherwise. This means quicker answers for patients and often better treatment plans. We’re seeing a big shift from how things used to be done to using smart, data-driven approaches.
Key Takeaways
- AI medical diagnosis tools use machine learning to analyze patient data, like images and health records, to help doctors identify diseases.
- These tools can improve how accurate diagnoses are and speed up the process, leading to faster treatment for patients.
- AI is being used in areas like radiology, pathology, and heart health to find problems earlier and more precisely.
- Integrating AI into hospitals means connecting it with current systems and making sure it’s easy for medical staff to use and trust.
- While AI offers many benefits, challenges like data bias and the need for clear rules still need to be worked out.
Understanding AI Medical Diagnosis Tools
Artificial intelligence is really changing how doctors figure out what’s wrong with people. Think of it like a super-smart assistant that can look at a ton of information way faster than any human could. These AI diagnostic tools are basically computer programs that have been trained on massive amounts of medical data, like X-rays, lab results, and patient histories. They learn to spot patterns that might indicate a disease or condition, sometimes even before a person has obvious symptoms. It’s a big shift from how things used to be done, where everything relied on a doctor’s personal experience and interpretation.
Defining AI Diagnostic Systems
At its core, an AI diagnostic system is a piece of software designed to help healthcare professionals identify illnesses. These systems use complex algorithms, often involving machine learning and deep learning, to sift through patient information. They’re built to recognize subtle clues within medical images, lab reports, or even patient-reported symptoms. The goal isn’t to replace doctors, but to give them a powerful tool that can process data with incredible speed and consistency. It’s like having a second opinion that’s available instantly and has reviewed millions of similar cases.
How AI Analyzes Patient Data
AI tools look at patient data in a few key ways. For medical images, like CT scans or MRIs, they use something called computer vision to analyze the pixels and identify anomalies – maybe a spot that looks suspicious or a fracture line. When it comes to lab results or patient records, AI can process text and numbers, looking for trends or deviations from the norm. It’s all about pattern recognition on a massive scale. For example, an AI might be trained on thousands of ECG readings to spot irregular heart rhythms that are easy to miss. The more data these systems process, the better they get at making accurate assessments. This ability to learn from data is what makes AI so powerful in medicine, allowing it to adapt and improve over time, much like how a doctor gains experience with each patient they see. We’re seeing AI being used to analyze everything from retinal scans to detect diabetic retinopathy to analyzing genetic sequences for predispositions to certain diseases.
AI Versus Traditional Diagnostics
When you compare AI to traditional diagnostic methods, the differences are pretty striking. Doctors have always relied on their training, experience, and diagnostic tools like stethoscopes or imaging machines. While incredibly effective, these methods can be time-consuming, and human interpretation can sometimes vary. AI, on the other hand, can process vast datasets in seconds, potentially reducing the time it takes to get a diagnosis. It can also offer a level of consistency that’s hard for humans to maintain, especially when dealing with fatigue or heavy workloads. Think about it: a radiologist might look at hundreds of scans a day. An AI doesn’t get tired. However, it’s important to remember that AI is a tool to assist, not replace. The human element of empathy, understanding a patient’s broader context, and making the final judgment call remains with the medical professional. It’s a partnership, really, where AI handles the heavy data lifting, allowing doctors to focus more on patient care and complex decision-making. The integration of AI into healthcare is a significant step, and understanding how these systems work is key to appreciating their potential impact on patient outcomes and the overall efficiency of medical practices. Companies are working to make these tools compatible with existing hospital systems, aiming for a smooth transition into everyday clinical use, and some are even developing mobile applications to extend these diagnostic capabilities to healthcare providers on the go. This move towards more accessible and integrated AI solutions is a major development in the field, promising to reshape how medical diagnoses are made and delivered. The future of healthcare is increasingly intertwined with advancements in artificial intelligence, and staying informed about these changes is important for anyone involved in the medical industry or simply interested in the evolution of health technology. The potential for AI to improve diagnostic accuracy and speed is immense, and it’s exciting to see how these technologies will continue to develop and be applied in the coming years, potentially leading to earlier disease detection and more personalized treatment plans for patients worldwide. The ongoing development in areas like natural language processing is also set to play a big role, allowing AI to better understand and interpret clinical notes and patient interactions, further refining its diagnostic capabilities. This evolution points towards a future where AI might not just diagnose but also suggest the most effective treatment paths, moving towards truly prescriptive healthcare solutions. The journey of AI in diagnostics is still unfolding, but its impact is already being felt across the medical landscape, offering a glimpse into a more efficient and precise future for healthcare.
Applications of AI in Medical Diagnosis
AI isn’t just a buzzword anymore; it’s actively changing how doctors figure out what’s wrong with people. Think about it – instead of just relying on a doctor’s experience, we now have smart systems that can sift through tons of information way faster than any human could. This means we’re getting better at spotting problems early and starting treatment sooner. It’s a pretty big deal for patient care.
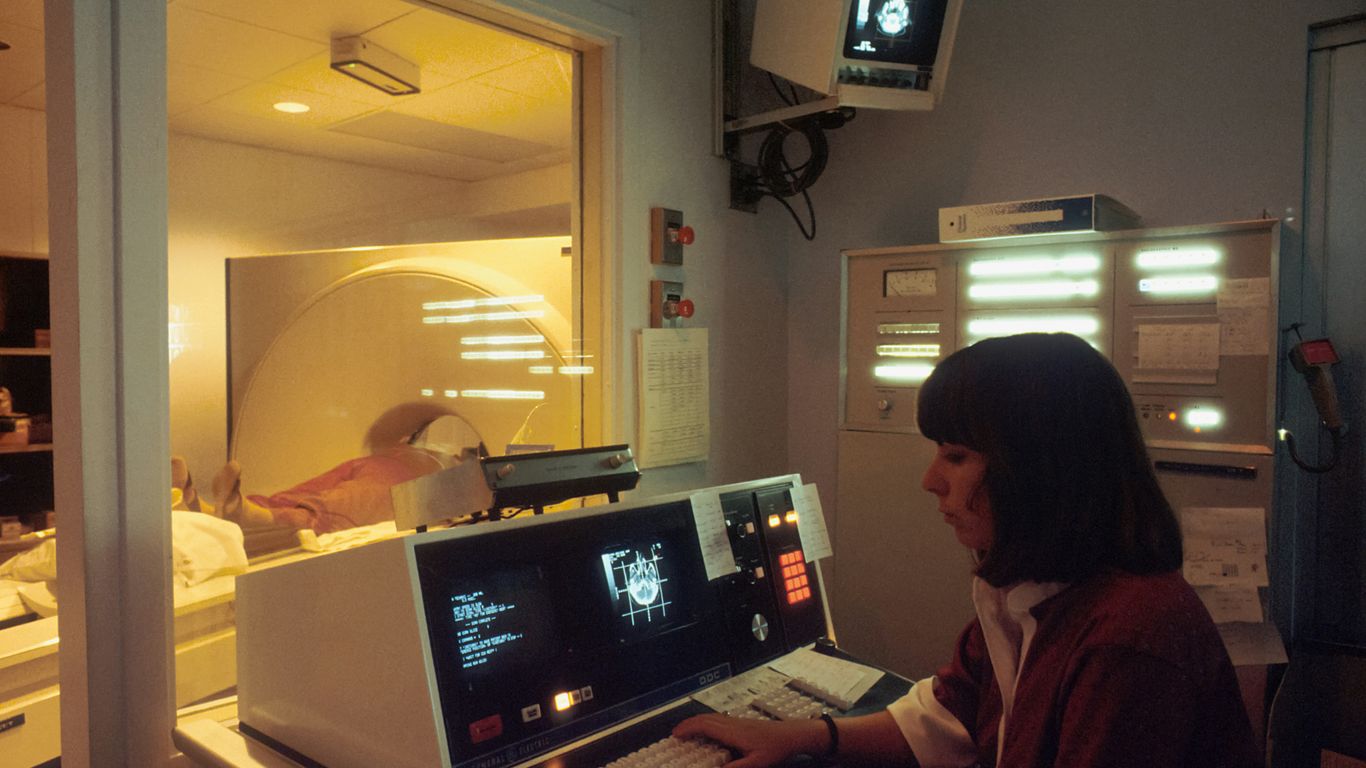
AI in Radiology and Pathology
Radiology and pathology are areas where AI is really shining. These fields rely heavily on looking at images, like X-rays, CT scans, MRIs, and tissue slides. AI, especially with its computer vision skills, can spot tiny details in these images that might be missed by the human eye. For example, AI models trained on thousands of mammograms have shown they can reduce both false positives and false negatives. Some studies even suggest AI can be more sensitive than radiologists in detecting certain cancers, like breast cancer, especially in its early stages. It’s like having a super-powered assistant for the folks who spend their days looking at scans and slides.
Cardiac Health and AI Analysis
When it comes to heart health, AI is also making waves. Analyzing things like EKGs and other heart imaging data can be complex. AI can process these signals and images to identify patterns that might indicate a risk for heart disease, sometimes even before symptoms show up. This ability to pick up on subtle signs is incredibly important for preventing serious cardiac events. It’s helping doctors get a clearer picture of a patient’s heart health and make more informed decisions about treatment and lifestyle changes.
AI for General Practice and Triage
Even in everyday doctor’s offices, AI is starting to help out. Think about initial symptom checks or deciding who needs to see a doctor most urgently. AI-powered chatbots or virtual assistants can ask patients about their symptoms and medical history. Based on this information, they can help guide patients on whether they need to make an appointment, go to the emergency room, or if they can manage their symptoms at home. This not only helps patients get the right care faster but also frees up doctors and nurses to focus on those who need immediate attention. It’s a way to make the whole process of seeking medical help a bit smoother and more efficient for everyone involved.
AI tools are not just about finding diseases; they’re about making the entire diagnostic process smarter and more accessible. By processing vast amounts of data quickly and spotting patterns humans might overlook, these systems are helping to catch illnesses earlier and more accurately. This shift means faster treatment plans and potentially better outcomes for patients, especially in complex fields like radiology and cardiology, and even in everyday primary care settings.
Key Advantages of AI Diagnostic Tools
AI diagnostic tools are really changing the game in healthcare. They’re not just fancy new gadgets; they bring some serious benefits that can make a real difference for both patients and doctors. Think about it – getting the right diagnosis faster and more accurately can mean everything when you’re dealing with a health issue. These tools are designed to help with that, making the whole process smoother and more effective.
Enhancing Diagnostic Accuracy
One of the biggest wins with AI is how it can spot things that might be missed otherwise. AI systems are trained on huge amounts of data, allowing them to pick up on subtle patterns in scans, lab results, or patient histories that even the most experienced human eye might overlook. This means catching diseases earlier, especially those tricky early stages or rare conditions, which is a massive step forward.
- Detecting subtle anomalies in medical images.
- Identifying patterns indicative of rare diseases.
- Reducing the likelihood of misdiagnosis due to human fatigue or oversight.
The ability of AI to process vast datasets and identify complex correlations means it can act as a powerful second opinion, bolstering confidence in diagnoses and potentially preventing serious conditions from going undetected.
Accelerating Diagnosis and Treatment
Time is often critical in healthcare. AI diagnostic tools can significantly cut down the time it takes to analyze information. Instead of waiting days for lab results or complex scan interpretations, AI can often provide insights in minutes. This speed allows doctors to start treatment sooner, which can lead to much better outcomes for patients. It also helps reduce the backlog in busy clinics and hospitals.
- Rapid analysis of imaging scans (X-rays, CTs, MRIs).
- Quick interpretation of laboratory results and patient data.
- Prioritizing urgent cases for immediate attention.
Scalability and Cost Efficiency
AI tools are incredibly scalable. Once developed, they can be deployed across many different healthcare settings, from large hospitals to smaller clinics, without needing a proportional increase in specialized staff. This is particularly helpful for areas that might not have access to a lot of medical specialists. Plus, by improving accuracy and speed, AI can help reduce costs. Fewer diagnostic errors mean fewer unnecessary tests or procedures, shorter hospital stays, and less administrative work, making the whole system more efficient and affordable.
| Benefit | Description |
|---|---|
| Scalability | Easily deployable across multiple facilities and patient populations. |
| Cost Reduction | Minimizes errors, redundant tests, and administrative overhead. |
| Accessibility | Extends diagnostic capabilities to underserved or remote areas. |
Integrating AI Medical Diagnosis Tools
So, you’ve got these amazing AI diagnostic tools, but how do you actually get them working in a real hospital or clinic? It’s not as simple as just plugging them in, you know. There’s a whole process to making sure they play nice with all the existing systems already in place. Think about all the patient records, lab results, and imaging data – it all needs to talk to the new AI software. Getting this right means the AI can actually access the information it needs to do its job effectively.
Seamless Integration with Existing Systems
Making AI tools work with what’s already there is a big deal. Most healthcare places use Electronic Health Records (EHRs), and that’s where a lot of patient info lives. The AI needs to be able to pull data from these EHRs, analyze it, and then maybe even put its findings back into the record. It’s like teaching a new employee how to use all the company’s old software. You want it to be smooth, not a constant headache. This also includes connecting with lab systems and imaging archives. If the AI can’t easily get to the X-rays or blood test results, it’s not going to be much help. The goal is to make the AI a natural part of the workflow, not an extra step that slows things down.
Extending Capabilities to Mobile Platforms
It’s not just about the big computers in the back office anymore. We’re seeing AI diagnostic capabilities showing up on phones and tablets. This is huge for doctors and nurses who are on the move. Imagine a doctor getting an alert on their phone about a critical finding in a patient’s scan, right when they need it. This kind of instant access means faster decisions, especially in emergencies. Wearable devices are also part of this, constantly collecting health data that AI can analyze in real-time Wearable devices enhance quality of life. It means healthcare can be more proactive, not just reactive.
Addressing Trust and Adoption Challenges
Okay, so the tech is there, but getting people to actually use it and trust it? That’s another story. Doctors and nurses have spent years training and developing their own instincts. They might be hesitant to rely on what a computer tells them, especially if it contradicts their own judgment. Building trust means showing them that the AI is a partner, not a replacement. It means making sure the AI’s reasoning is clear, so they understand why it’s suggesting something. Transparency is key here. Plus, there’s the training aspect – making sure everyone knows how to use the tools properly and understands their limitations. It’s a gradual process, but as people see the benefits, like catching things earlier or saving time, adoption usually follows.
The real challenge isn’t just the technology itself, but how it fits into the human side of healthcare. It’s about making sure these powerful tools support, rather than disrupt, the patient-doctor relationship.
Real-World Impact of AI Diagnostic Tools
It’s pretty amazing to see how AI is actually being used in hospitals and clinics right now, not just in theory. These tools are starting to make a real difference in how doctors and nurses do their jobs and, more importantly, how patients get treated. We’re talking about systems that can look at scans and data way faster than a person can, spotting things that might otherwise be missed. This isn’t science fiction anymore; it’s becoming part of everyday patient care.
Case Studies: IBM Watson and Aidoc
When you hear about AI in healthcare, IBM Watson often comes up, especially in cancer treatment. Watson’s AI looks at a patient’s medical history, genetic makeup, and a huge amount of medical research to suggest treatment plans. It’s like having a super-smart assistant that’s read every medical journal ever published. Then there’s Aidoc, which is a big help for radiologists. Their AI software scans medical images, like CT scans, and flags anything that looks urgent, such as a brain bleed or a collapsed lung. This helps doctors prioritize which patients need immediate attention, cutting down on delays when every second counts.
Zebra Medical Vision’s AI Platform
Zebra Medical Vision has developed a platform that uses AI to analyze medical images for a variety of conditions. Think of it as a second pair of eyes for doctors looking at X-rays, CT scans, or MRIs. Their AI can identify early signs of diseases like osteoporosis, fatty liver disease, or even certain types of cancer from routine scans. This means conditions can be caught much earlier than they might have been otherwise, potentially leading to better outcomes for patients. The platform is designed to integrate with existing hospital systems, making it easier for them to adopt this new technology.
AI’s Role in Early Disease Detection
One of the most significant impacts AI is having is in catching diseases early. By analyzing vast amounts of patient data, including images, lab results, and even genetic information, AI can identify subtle patterns that might indicate the presence of a disease long before symptoms become obvious. This early detection is a game-changer for many illnesses, particularly cancers and chronic conditions. It allows for timely intervention, which often leads to more effective treatment and improved survival rates. The ability of AI to sift through complex data sets and highlight potential issues is transforming preventative care and patient outcomes.
The Future of AI in Healthcare Diagnostics
So, what’s next for AI in figuring out what’s wrong with people? It’s pretty exciting, honestly. We’re moving beyond just spotting problems to actually predicting them before they even start. Think about AI looking at your genes, your habits, and even what’s going on in the environment around you to give you a super-specific health picture. It’s like having a crystal ball, but for your well-being.
Predictive Analytics and Personalized Medicine
This is where things get really interesting. AI is getting better at crunching huge amounts of data – not just your medical history, but also lifestyle factors and genetic makeup. This allows for what we call predictive analytics. Instead of just reacting to illness, AI can help us anticipate it. For example, it might flag someone as having a higher risk for a certain condition years in advance, giving doctors a chance to intervene early. This is a big step towards truly personalized medicine, where treatments are tailored to the individual, not just the disease.
Advancements in Natural Language Processing
Doctors write a lot of notes, right? And a lot of that information is just text, not neatly organized data. That’s where Natural Language Processing (NLP) comes in. AI is getting much better at reading and understanding these doctor’s notes, patient interviews, and other unstructured text. It can pull out key details that might otherwise be missed, adding another layer to the diagnostic puzzle. This means AI can understand the nuances of a patient’s story, not just the numbers.
AI’s Move Towards Prescriptive Solutions
Right now, AI is mostly used for diagnosis – telling you what’s wrong. But the next big leap is for AI to tell you what to do about it. We’re talking about prescriptive solutions. So, not only will AI identify a condition, but it will also suggest the best treatment plan, considering all the personalized data we talked about. It’s like having a super-smart assistant that not only diagnoses but also advises on the cure. This could really change how quickly and effectively we treat people, making healthcare more proactive and efficient. It’s a future where technology helps us stay ahead of illness, much like how driverless cars are changing transportation [8d18].
The evolution of AI in diagnostics is pushing healthcare towards a more proactive and individualized approach. By analyzing complex datasets and understanding nuanced patient information, AI is set to become an indispensable partner in predicting, diagnosing, and treating diseases.
Challenges and Considerations for AI Tools
While AI medical diagnosis tools promise a lot, getting them to work smoothly in real healthcare settings isn’t always straightforward. There are a few big hurdles we need to think about before these tools become standard practice. It’s not just about the tech itself, but how it fits into the human side of medicine too.
One of the trickiest parts of AI is making sure the data it learns from is fair. If the data used to train an AI model doesn’t represent everyone equally, the AI can end up making biased decisions. For example, if an AI was trained mostly on data from one demographic group, it might not work as well for people from other groups. This could lead to some patients getting less accurate diagnoses simply because the AI wasn’t trained on data that included them properly.
- Data Source Diversity: Training data needs to come from a wide range of hospitals, patient types, and geographic locations.
- Algorithmic Auditing: Regularly checking AI models for biased outputs is important.
- Bias Mitigation Techniques: Developing methods to actively correct for bias during the AI’s learning process.
The risk of AI amplifying existing societal biases is a serious concern. If not carefully managed, these tools could inadvertently worsen health disparities rather than help close them.
Getting AI tools approved and used consistently across different healthcare systems is another challenge. There aren’t always clear rules or standards for how these tools should be built, tested, and used. This can make it hard for hospitals to know which tools are reliable or how to integrate them safely. Plus, regulations need to keep pace with how fast the technology is changing.
- Developing Clear Guidelines: Regulatory bodies need to create straightforward rules for AI in healthcare.
- Interoperability Standards: Making sure different AI tools and existing hospital systems can talk to each other.
- Performance Benchmarking: Establishing common ways to measure how well AI diagnostic tools perform.
Medical data is incredibly sensitive. When AI tools use this data, we have to be extra careful to protect patient privacy and prevent data breaches. This means having strong security measures in place and being transparent about how data is being used. Patients need to feel confident that their personal health information is safe.
- Robust Cybersecurity: Implementing advanced security to guard against unauthorized access.
- Data Anonymization: Removing personal identifiers from data used for training and analysis.
- Patient Consent and Transparency: Clearly informing patients about how their data might be used by AI systems.
The Road Ahead
So, where does all this leave us? AI in medical diagnosis isn’t just a futuristic idea anymore; it’s here, and it’s changing things fast. These tools can spot problems quicker and more accurately than we often can, which means faster treatment for patients and less stress on our doctors and nurses. Think about getting a diagnosis in minutes instead of days, or catching a disease before it even shows obvious symptoms. It’s a big deal. Of course, it’s not all smooth sailing. We need to make sure the data used to train these AI systems is fair and doesn’t leave anyone behind, and we need clear rules for how they’re used. Plus, building trust between doctors and these new AI helpers is key. But the potential is huge. As AI gets smarter and we get better at using it, healthcare is going to become more precise, more efficient, and hopefully, more accessible for everyone. It’s an exciting time to see how this technology continues to shape how we stay healthy.