Siloed healthcare is a term you hear a lot, but what does it really mean for patients and the system as a whole? In simple terms, it’s when different parts of the healthcare system work on their own, without much connection to each other. This can make it tough for people to get the care they need, especially when their health issues are complex or ongoing. Let’s take a closer look at why these silos exist, how they affect patients, and what can be done to make healthcare more connected.
Key Takeaways
- Siloed healthcare happens when different teams, departments, or organizations don’t share information or work together well.
- Patients often experience repeated tests, mixed messages, and delays because their care isn’t coordinated across providers.
- Money and management structures in healthcare can make silos worse, as each group focuses on its own goals and budgets.
- Technology can help, but only if systems are set up to talk to each other and share patient information safely.
- Breaking down silos requires leadership, changes in how care is organized, and a focus on making things easier for patients.
The Roots of Siloed Healthcare in Modern Systems
Historical Development of Healthcare Silos
Siloed healthcare didn’t happen overnight. It’s a patchwork that formed over decades as health systems grew and specialties multiplied. As care moved from the local general practitioner toward bigger hospital systems, more departments were created—each with their own leaders, priorities, and ways of working. Beyond just departments, the funding and governance structures in many countries—like Medicare in the US and similar health programs in Australia and the UK—grew separately, making different sectors responsible for their own budgets. That means hospitals, clinics, community services, and even private providers often have little reason (or ability) to communicate or coordinate their activities. So, even when better coordination means savings for the whole system, individual units might not see the benefit in breaking down their own walls. You can see more about how information silos hurt innovation in data silos in healthcare.
Impact of Social Identity and Professional Boundaries
It’s easy to think it’s just a technology, policy, or funding problem, but there’s a huge human element, too. Professional identity kicks in early—medical students, nurses, specialists, and administrators all learn the “right” way to think and work in their corner of the system. Over time, these boundaries grow thicker.
- Strong in-group thinking forms during training and specialization
- Departments focus on optimizing their own results instead of the big picture
- Without trust or familiarity between groups, collaboration falls flat
Often, this “us versus them” mindset is so built-in that folks barely realize it’s happening. It’s not just about territory—it’s about habits, power, and who gets the say in decisions.
Governance Structures Reinforcing Fragmentation
The way healthcare systems are managed often makes silos even stronger. Governance is split between federal, state, local, and sometimes private actors, all with their own rules and goals. Instead of everyone working with the same playbook, each group scraps for its own share of funding and influence. A few concrete effects show up again and again:
- Patchwork of funding sources, each with conflicting priorities.
- Policies and regulations designed to protect one silo can accidentally block system-wide communication.
- Everyone’s focused on proving their unit’s value, rather than improving outcomes for patients across the board.
So it’s not just history or money—it’s the daily push and pull between different groups and priorities that keeps silos standing tall.
Barriers to Integrated Patient Care Created by Siloed Healthcare
Healthcare silos make it tough for patients to move easily through the system. From chopped-up communication to a sense of isolation among staff, these divisions add up over time.
Communication Breakdowns and Information Gaps
It’s not surprising—when different teams or departments don’t talk regularly, misunderstandings happen. Key patient info can slip through the cracks, which leads to mistakes or delays. Hospitals and clinics often use different systems and tools for sharing updates, if they share them at all. This means:
- Test results might not get to the doctor who needs them most.
- Patients might have to repeat their story over and over.
- Clarity can get lost as everyone works with partial details.
Here’s how these issues can break down in daily practice:
| Scenario | Possible Outcome |
|---|---|
| Missed handoff note | Medication error or delay |
| Unshared diagnostic result | Unnecessary repeat imaging |
| Lack of follow-up instructions | Patient confusion post-discharge |
Loss of Care Continuity and Patient Experience
When each department operates separately, patients can feel like they’re bouncing around with no one really in charge. It’s easy for details to be lost from one hand to the next. This means:
- Patients might not know which provider to ask about next steps.
- Follow-ups can fall through, especially after hospital stays.
- Transitions (from one doctor or team to another) are often disconnected and rushed.
The end result? Many people have to advocate fiercely for themselves, just to get the attention or care they need. Some simply give up.
Organizational Culture and Silo Mentality
In some healthcare organizations, it feels like every unit is its own little world. People get caught up focusing on their piece of the puzzle, ignoring the bigger picture. Barriers are reinforced by:
- A protective mindset about resources and knowledge (“that’s not my department”)
- Leadership that doesn’t encourage working across teams
- Training and social identity built around loyalty to a specific professional group
Staff can end up mistrusting other teams, which only makes things harder for patients. Over time, this mentality makes change—even simple improvements—feel impossible. And ultimately, everyone loses out, patients most of all.
Financial and Organizational Factors Sustaining Siloed Healthcare
Healthcare silos don’t just happen because of human habit—they’re shaped and kept in place by the way money moves between departments, how organizations make decisions, and what different groups actually want to achieve. If you follow the cash flow and management structures, the reason for siloed systems becomes pretty obvious.
Budgetary Separation and Conflicting Incentives
Most hospitals and healthcare networks split their budgets, so each department keeps close control over its own funds. That means a win for one department may actually be a loss for another. For example, an emergency department might avoid referring patients to community care since their budgets are totally separate. Instead of seeing the whole patient journey, these silos keep their focus narrow and self-serving.
Key problems with budgetary separation include:
- Individual units hesitate to share resources, leading to hoarding instead of collaboration
- Departments often ignore opportunities to improve the entire system because they’re evaluated on their own costs and results
- Short-term financial goals usually beat out long-term patient benefits
| Department | Budget Managed Separately | Collaboration Incentive | Typical Result |
|---|---|---|---|
| Emergency | Yes | Low | Silos |
| Surgery | Yes | Low | Silos |
| Community Care | Yes | Low | Silos |
Fragmented Funding Models Across Care Settings
Different areas of healthcare—primary, specialty, community-based, and hospital—are usually funded by distinct government or private sources. That means health professionals can be on totally different payment plans and value systems, even when they’re working with the same patients.
Here are a few ways fragmented funding creates silos:
- Payment structures reward volume over coordination (e.g., fee-for-service for doctors means more visits, not necessarily better care)
- Funding for chronic disease management often runs separately from acute care funding, stalling care integration
- Technology budgets are rarely joined up, increasing the odds for digital silos
There’s more information on how organizational barriers affect cooperation in integrated partnerships in this study about collaborative integration.
Stakeholder Interests and Diffusion of Responsibility
Every part of the health system, from front-line clinicians to managers and external organizations, has its own set of priorities. Sometimes, these don’t line up. When something goes wrong with a patient, there’s a tendency for nobody to take the blame. The bigger and more complex the system, the more likely that finger-pointing and buck-passing is baked in:
- No single group feels responsible for the overall patient experience
- Stakeholders focus energy on their own goals
- Resources get wasted through duplicated efforts or gaps in service
The bottom line? Until the flow of money and the way groups are organized changes, it’s tough to break out of the habit of siloed care. Connected, patient-focused systems will remain out-of-reach if decision-makers don’t address these organizational and financial walls.
The Role of Technology and Data in Perpetuating Silos
Most people believe technology should be the key to bringing healthcare together, but it often does the opposite—it keeps parts of the system apart. There’s a lot to unpack on why that is, but it boils down to the ways our tech, data, and systems have developed in isolation. Rather than providing smooth support, tech can put up barriers, keeping providers and patients separated by screens and paperwork. Let’s break down some core reasons why this happens.
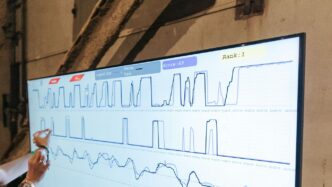
Challenges of Interoperability Between Systems
Ever tried transferring your health information from one doctor to another? Not easy, right? That’s because different Electronic Health Record (EHR) vendors build their own systems with their own rules, making integration complicated and expensive. Some of the main hurdles in interoperability include:
- Different hospitals and clinics use software that can’t easily talk to each other.
- Custom-built systems at specific locations may not follow the same standards.
- Security protocols and privacy regulations make sharing information even trickier.
Basically, when systems don’t play nice together, information gets lost, delayed, or stays siloed. If you want to see this in action, just look at how wearable technology faces data consistency and privacy challenges—these same problems echo through the whole healthcare system.
Health Data Fragmentation and Access Issues
Fragmentation of health data is one of the biggest headaches for both patients and professionals. Your test results, medication lists, treatment histories, and more end up scattered across numerous databases. This happens due to:
- New tech tools introduced without replacing outdated ones.
- Separate record-keeping by labs, specialists, and primary care doctors.
- Patients using mobile health apps or devices that don’t sync with hospital records.
The result? Health data lives in multiple places, and sometimes, even you can’t access your entire history without serious effort.
| Consequence | Description |
|---|---|
| Incomplete information | Providers miss key facts during appointments. |
| Repeated paperwork | Patients re-enter the same details often. |
| Potential for mistakes | Lack of full history leads to errors. |
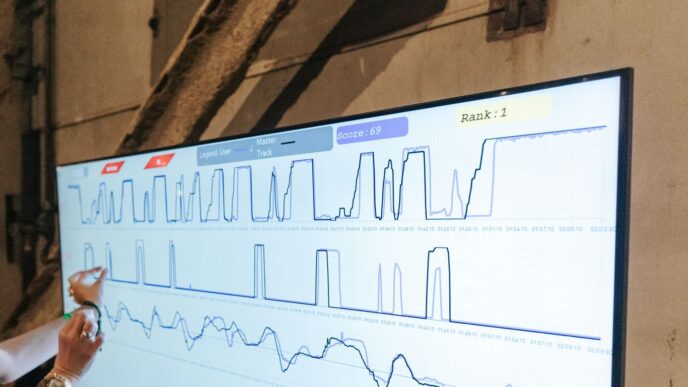
The Limitations of Electronic Medical Records
Electronic Medical Records (EMRs) were supposed to make life easier. Ironically, they’ve often made it more frustrating. Here’s why EMRs haven’t solved the problem of healthcare silos:
- Each EMR has its own data standards, so migration and sharing are a pain.
- Clinicians spend more time on data entry than seeing patients, which can reduce communication among care teams.
- EMR companies sometimes "lock in" data, making it hard to switch vendors or share data widely.
Some organizations have tried to use workarounds or extra data-sharing platforms, but these just add more layers and confusion. At the end of the day, without a unified approach, EMRs can add to the noise instead of making things simpler.
In short, the promise of technology fixing all of healthcare’s problems hasn’t come true. Until we address interoperability, fragmented data, and the quirks of EMRs, silos will stick around—and patients will keep feeling the friction.
Patient Consequences of Siloed Healthcare Approaches
Care Coordination Failures and Health Outcomes
When healthcare organizations work in silos, patients often experience a lack of coordination between services. This can show up as confusing handoffs or missed follow-ups, which impact health outcomes in very real ways. For example, a specialist may change a medication but not update the primary care doctor, leading to unsafe drug combinations. Patients with multiple chronic conditions are especially at risk when their care isn’t connected.
- Missed test results and duplicate assessments
- Delays in necessary treatments
- Unclear responsibility for managing ongoing conditions
Here’s a quick table showing how coordination issues can impact outcomes:
| Scenario | Possible Result |
|---|---|
| Lab results not shared | Delayed diagnoses |
| Discharge summary missing | Incomplete transition to rehab |
| Medication change unreported | Adverse drug reactions |
Patient Disempowerment and Decision-Making Challenges
Patients often feel lost in a system marked by fragmented care. Each department tends to focus only on its area, leaving patients to bridge the gaps. They may be forced to repeat their history over and over or choose between conflicting advice from different providers. The burden of coordinating appointments and understanding next steps falls on the patient, not the system.
- Overwhelming information and medical jargon
- Difficulty knowing who to contact for help
- Anxiety and frustration with the care journey
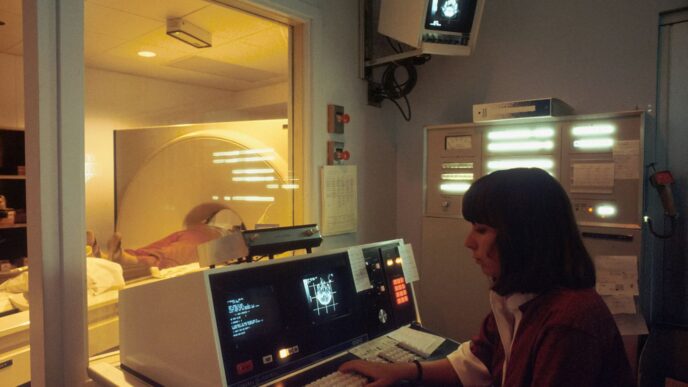
Redundant Testing and Delayed Treatments
One of the direct effects of silos is unnecessary repetition. Different providers might order the same bloodwork or scans simply because previous results were never shared. This wastes time, increases costs, and can put patients at risk (like extra exposure to radiation from repeat imaging). Even worse, patients sometimes have to wait longer for needed treatment because of hold-ups in transferring information or finalizing referrals between departments.
- Duplicate lab tests or imaging
- Treatment plans stalled waiting for records
- Financial costs passed to patients or insurers
People come to healthcare for help — but, too often, the system’s internal walls get in the way of what matters most: better health.
Strategies for Overcoming Siloed Healthcare and Achieving Integration
Moving past siloed healthcare isn’t just some trendy idea—it’s about making sure patients don’t fall through the cracks. It might sound simple, but taking down these barriers can be tough. Here’s how organizations are working to connect the dots and make things actually work together.
Leadership and Governance Innovations
Real change in healthcare integration comes from leadership that refuses to stick with the status quo. Leaders must set clear expectations around teamwork and accountability. Often, this means:
- Setting shared goals and objectives across all departments
- Creating joint leadership councils with representatives from different care settings
- Making people responsible for patient outcomes together—not just in isolation
Effective governance will also look at how local communities and stakeholders can be involved. For example, some health systems set up governing boards with hospital managers, primary care reps, and even patient advocates all sitting at the same table. This way, decision-making reflects broader needs and not just internal politics. Sometimes these efforts use structures like Collaborative Commissioning, where savings and efficiency gains are reinvested locally, creating a positive feedback loop. For more detail on how leadership approaches reinforce fragmentation or integration, see impact of healthcare data silos.
Adopting Integrated Care Models
Changing care models is one of those things that sounds neat on paper, but it’s a messy job in reality. Healthcare systems are experimenting with integrated teams that cut across specialties—think doctors, nurses, and social workers collaborating instead of working in their own bubbles. Integrated care models generally involve:
- Patient-centered care plans shared between providers
- Regular interdisciplinary case conferences
- Coordinators who follow patients across all sites and services
Organizations adopting these approaches often report greater patient satisfaction and fewer readmissions. Still, the devil is in the details—rolling out these models demands extra training, rule changes, and the willingness to challenge traditions.
Leveraging Technology for Seamless Information Flow
If you want everyone on the same page, you’ve got to fix data barriers. The main stumbling blocks here are incompatible software systems and limited access to crucial info. Here’s how some healthcare systems are working to break open silos with tech:
- Interoperable systems that allow records to move between clinics, hospitals, and specialists
- Centralized data storage and controlled access so the right provider sees what they need, when they need it
- Automation tools to cut down on duplicate data entry and reduce errors
Let’s take a quick look at a simple table showing common tech-related strategies:
| Strategy | Main Benefit |
|---|---|
| Interoperable Health IT | Quicker info sharing |
| Centralized Data Access | Fewer lost records |
| AI and Automated Data Management | Less manual work |
Many places still wrestle with electronic medical records that just don’t talk to each other, so it’s a work in progress. It’s not just about getting new gadgets—it’s about policy, training, and old-fashioned communication. A better technology setup can open up collaboration, make transitions smoother, and help patients receive better care.
In the end, moving beyond silos in healthcare takes bold leadership, new care models, and smarter use of technology. The solutions aren’t magic bullets, but they’re steps in the right direction.
Conclusion
Siloed healthcare is a problem that most people working in the system have seen up close. It shows up as confusion, delays, and sometimes even worse outcomes for patients. The reasons for these silos are complicated—everything from funding to professional identity to old habits. But at the end of the day, it’s patients who feel the impact the most. While there’s no magic fix, small steps like better communication, shared goals, and putting the patient at the center can start to break down these walls. It’s not easy, and it won’t happen overnight, but if everyone—from doctors to administrators to policymakers—keeps pushing for more connected care, things can get better. The hope is that, over time, healthcare can become less about separate parts and more about working together for the people who need it most.
Frequently Asked Questions
What does ‘siloed healthcare’ mean?
Siloed healthcare means different parts of the health system work separately instead of together. For example, hospitals, clinics, and specialists might not share information or work as a team, which can create problems for patients.
Why is it hard for healthcare teams to share information?
It can be hard because each group often uses its own system for storing patient information. These systems might not connect well with others, making it tough to share important details quickly and safely.
How does siloed healthcare affect patients?
When healthcare is siloed, patients might have to repeat their medical history, get the same tests more than once, or wait longer for treatment. It can also make it harder for them to understand their care plan and feel in control of their health.
What causes healthcare to become siloed?
Healthcare becomes siloed because of things like separate budgets, different rules, and strong group identities among doctors and nurses. Sometimes, leaders and organizations focus only on their own goals, not on working together with others.
Can technology help fix siloed healthcare?
Yes, technology can help by making it easier to share information. For example, better computer systems and secure ways to send data can help doctors and nurses work together. But, these systems need to be able to ‘talk’ to each other, which is still a challenge.
What are some ways to make healthcare more connected?
Healthcare can be more connected if leaders encourage teamwork, if organizations use systems that share information easily, and if everyone focuses on the patient’s needs first. New care models and better use of technology can also help break down silos.