AI in medical diagnostics is changing the way doctors find and treat diseases. Instead of just relying on what they see or know, doctors can now use computer programs to look at lots of patient data—like X-rays, blood tests, and even genetic info. These tools can spot patterns that humans might miss, sometimes catching problems earlier or helping pick the right treatment faster. Things are moving quickly, and while there are still some bumps in the road, AI is starting to make healthcare more accurate and efficient for everyone.
Key Takeaways
- AI in medical diagnostics can help doctors find diseases sooner by looking at patterns in images and test results.
- Using AI, healthcare teams can create treatment plans that are more personalized to each patient’s needs.
- AI tools can cut down on mistakes in busy places like emergency rooms and help hospitals use their resources better.
- New technologies, like quantum computing and cloud systems, are making AI even faster and more powerful for medical diagnostics.
- It’s important to address fairness, privacy, and trust so that everyone can benefit from AI in healthcare.
Transforming Disease Detection with AI in Medical Diagnostics
AI is shaking up how doctors figure out what’s wrong with people. Long gone are the days when doctors relied only on what they could see or what traditional lab results showed. With machine learning and smart algorithms, disease detection has become faster, more accurate, and often picks up problems earlier than before.
Harnessing Machine Learning for Early Disease Identification
Catching illnesses before they progress is no longer just wishful thinking—it’s becoming reality thanks to machine learning. Here are a few ways AI is showing up in early identification:
- Complex models quickly sort through symptoms and lab results, flagging unusual patterns that might mean trouble.
- AI systems are often better than humans at picking out rare cases, such as certain cancers or infections, by comparing new patient data to massive databases.
- Practically, this means more people get prompted for follow-up exams or preventive care before symptoms get serious.
Here’s a look at results from a recent AI breast cancer screening study:
| Method | False Positives Reduction | False Negatives Reduction |
|---|---|---|
| AI Interpretation | 5.7% | 9.4% |
| Human Interpretation | – | – |
The numbers speak for themselves—AI doesn’t just guess, it tends to catch what humans might miss.
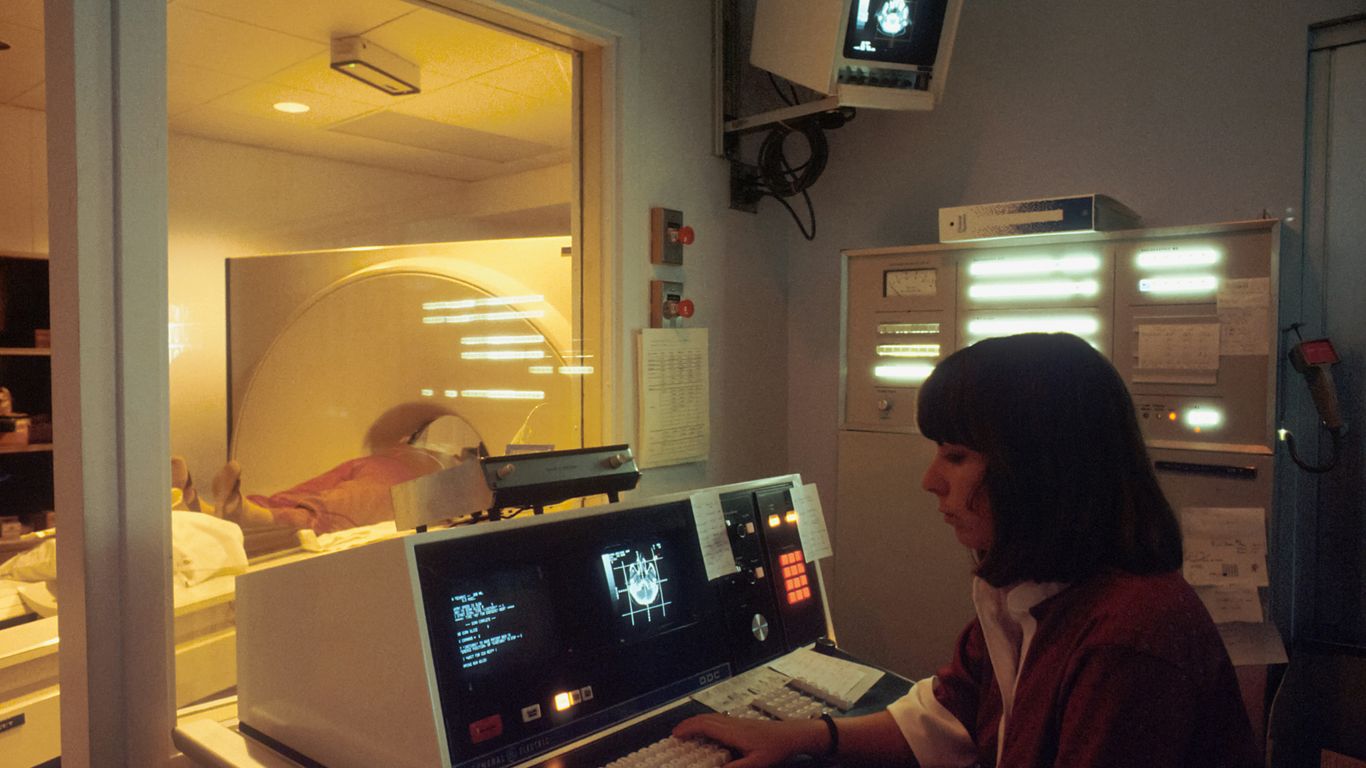
AI’s Impact on Imaging: X-rays, MRIs, and Beyond
Medical imaging is one area where AI has made a huge difference. Processing X-rays or MRIs by hand takes time and can be inconsistent from one radiologist to another. AI, on the other hand:
- Can examine thousands of images quickly, spotting tumors, fractures, or unusual growths with impressive speed.
- Is used in real-world systems—sort of like how complex pattern recognition helps detect pedestrians in cars—to scan for specific disease features, such as lung nodules or diabetic eye changes.
- Algorithms are constantly learning, so every scan they review helps make the next diagnosis even better.
Some recent studies show that, for certain problems like breast or skin cancer, AI can pick up warning signs earlier and sometimes with greater accuracy than the average specialist. That has potential to change the whole experience for patients and providers.
Analyzing Multimodal Data for Enhanced Diagnostic Accuracy
It’s not just images—AI is able to process all kinds of patient information at once. That might include:
- Electronic health records
- Lab results and vital signs
- Doctors’ notes
- Genomic or genetic information
By pulling together these pieces, AI builds a bigger, more detailed picture, and connects dots that ordinary software or humans might overlook. For example, mixing genetic data with imaging and clinical notes has helped spot early warning signs of complex diseases like heart troubles or autoimmune issues.
In a nutshell, AI for diagnostics isn’t just hype. It’s changing how medicine works day-to-day, helping doctors catch things earlier, more reliably, and with better odds for the patient.
Personalized Medicine and Predictive Analytics in Diagnostics
There’s a lot happening with AI in medicine, but where it really gets interesting is in how it makes healthcare personal—down to your genes, your past, and even your daily habits. AI-driven tools are now doing more than just broad predictions; they’re putting patient specifics at the center of diagnostics. Let’s unpack how it’s happening in three key ways.
Tailoring Treatment Plans Through Patient-Specific Insights
We all know that no two patients are alike. Now, medical diagnostics can actually reflect that. AI models use patient data—from past test results to current symptoms and even info from wearables—to recommend the best treatment plans for each person.
For example, doctors can:
- Compare data across thousands of similar patient profiles
- Identify which drugs are likely to work best for you
- Adjust dosages or therapies based on your unique response
Wearable devices also play a big role here. By tracking vital signs or activity in real time, they feed new data back into these models so treatments can be fine-tuned as you go.
Leveraging Genomic Data for Precision Diagnostics
AI is making it possible to use your genetic info to spot problems early and get the right diagnosis faster. When doctors plug genetic data into AI systems, these models can pick up patterns that suggest you might respond well—or poorly—to certain drugs, or that you may have a hidden risk of disease before symptoms show up.
Some big wins for AI with genomic data:
- Finding cancer subtypes that help decide on targeted therapies
- Predicting drug reactions (reducing trial and error)
- Matching rare diseases to patients based on gene mutations
Table: How Genetic Data Informs Diagnosis
| Genetic Info | Possible Outcome | AI Application |
|---|---|---|
| Cancer gene panels | Cancer subtype ID | Therapy selection |
| Pharmacogenomics | Drug metabolism prediction | Dose adjustment |
| Rare mutation info | Disease matching | Early diagnosis |
Predictive Modeling for Disease Progression and Risk Assessment
AI-powered predictive analytics may sound fancy, but at its core, it tries to answer questions like: "Who’s going to get sick, and when?" or "How soon might this disease get worse?". These models look at tons of variables: your age, medical history, habits, lab tests, and so on.
Here’s how predictive analytics gets used in real life:
- Flagging patients at high risk for problems like readmission after surgery
- Notifying care teams before chronic diseases escalate
- Supporting decisions on how often follow-ups should happen
Healthcare systems are now testing out these tools on everything from early heart disease warnings to predicting which cancer patients are most likely to benefit from extra monitoring. The best results tend to show up when AI has access to high-quality, regularly updated data, both from clinical visits and devices you use every day.
So, the future of diagnostics isn’t just about smarter machines—it’s about using them to figure out what’s most likely to work for each of us, personally.
Improving Clinical Workflow and Efficiency with AI
Artificial intelligence is finding its place on the frontlines of healthcare, not just behind the scenes. It’s starting to speed up tasks, cut down on mistakes, and make daily operations run more smoothly. These changes are already popping up in hospitals and clinics and they’re hard to ignore.
Reducing Diagnostic Errors in Emergency Settings
Emergency rooms get hectic fast. Every minute, doctors are dealing with patients who might have life-threatening conditions, and sometimes there’s just not enough information. AI-driven tools can now scan through electronic health records, vitals, and test results almost instantly. They pick up subtle warning signs that humans might overlook, like early symptoms of sepsis or signs of a stroke tucked away in labs or notes. AI can flag high-risk patients so clinicians can focus on the most urgent cases.
- AI can suggest potential diagnoses based on symptoms and risk profiles.
- Real-time alerts notify staff of abnormal lab or monitoring results.
- Predictive models estimate which patients might need intensive care soon.
This isn’t about taking the human out of medicine—it’s about giving doctors and nurses a head start when the situation is stressful and time is short.
Optimizing Resource Allocation with Real-Time Data
Hospitals are always juggling resources—beds, staff, equipment. When things get busy, knowing where to send people or which rooms should be ready is tricky. AI tracks patient flow and predicts admission surges by analyzing:
| Factor Analyzed | AI Output | Decision Influenced |
|---|---|---|
| ER admission rates | Predicted surges | Adjust staffing levels |
| Lab test volumes | Workflow bottlenecks | Change lab scheduling |
| ICU bed occupancy | Demand projections | Prioritize discharges/admissions |
- AI models can spot patterns in admissions, so staff aren’t caught off guard.
- Equipment involves a lot of tracking; smart systems know where machines and supplies are, which avoids unnecessary delays.
- AI-powered scheduling systems help keep the balance and avoid staff burnout.
Streamlining Radiotherapy and Laboratory Testing
Preparing cancer patients for radiotherapy is usually a painstaking process, especially when clinicians have to mark out tumors in scan images by hand. New AI software can draw these boundaries automatically, often in just a fraction of the time.
- Manual image segmentation can take hours for each patient. AI can drop that time to just minutes, which means people start their treatment sooner.
- Automated AI testing in labs sorts samples, flags abnormal results, and even reroutes questionable tests for review. This speeds up reporting and reduces lab errors.
- Teams can focus more on cases that really need a human look, instead of being bogged down with routine checks.
What’s next? More of these systems will probably show up in all sorts of departments, making it less about catching up with work and more about staying ahead. For busy doctors, nurses, and lab techs, it’s a relief. For patients, it could mean shorter waits and better care.
Emerging Technologies Shaping the Future of AI in Medical Diagnostics
It feels like every year, something new pops up in the world of AI diagnostics. Lately, the buzz has been about more powerful AI approaches, from quantum computers to general AI, and smarter ways of dealing with all the data pouring in from hospitals and clinics.
Quantum AI: Accelerating Diagnostic Capabilities
Quantum AI isn’t just a fancy term—it’s a possible game changer. At its core, quantum computing handles data in a way that old-school computers just can’t match. That means running AI models much faster and processing way more information at once.
Some things quantum AI could change in diagnostics:
- Sifting through millions of medical records in seconds
- Spotting rare disease patterns that take ordinary computers weeks
- Optimizing treatment choices based on complex data
When it comes to quick decision-making in healthcare, being faster and more precise could actually save lives.
| Technology | Potential Impact | Example Use |
|---|---|---|
| Quantum AI | Super-fast data analysis | Real-time outbreak detection |
| Conventional AI | Faster than manual, but slower for big data | Image review, test result sorting |
General AI for Complex Pattern Recognition
General AI (sometimes called AGI) is more like a smart helper than a single-purpose tool. Unlike today’s narrow systems, which flag one disease or highlight an abnormal image, general AI learns across lots of topics, making connections that aren’t always obvious even to experts.
Some possible benefits:
- Diagnosing conditions that have confusing or overlapping symptoms
- Noticing trends across a hospital (like infection spreading)
- Giving doctors suggestions backed by loads of historic and real-time patient data
Projects like DeepMind, Watson, and DeepQA are all racing to build these broad-thinking systems, and healthcare is a top target.
Integration of Edge and Cloud Computing in Diagnostics
Medical AI doesn’t just live in giant servers anymore. Increasingly, there’s a push to mix edge computing (little computers right at the patient’s bedside or even built into devices) with cloud data centers (the massive remote ones).
Here’s how this mix is starting to change things:
- Edge devices can check data like heart rate or scan results instantly, without waiting for the internet
- Large cloud systems pull all the data together for deeper analysis
- If one system goes down, the other can keep working—reducing disruptions
A simple breakdown:
- Edge for speed and privacy
- Cloud for big-picture analysis
- Both working together for smoother, safer diagnostics
It’s not perfect yet—there are hiccups with sharing info and matching up formats, but that’s being worked on.
In short, the future of diagnostic AI looks a lot more connected and fast, with smarter helpers and powerful new tech inside doctors’ toolkits. It’s exciting, if a little overwhelming to keep up with the pace of it all.
Ethical Considerations and Equitable Implementation of AI Diagnostics
Making AI in medical diagnostics work for everyone doesn’t just happen by itself. It takes careful planning, plenty of oversight, and some blunt conversations about data, fairness, and trust. Below, I’ll explore three big things that need serious attention: bias in AI, keeping patient data safe, and making sure the rules are clear for everyone.
Addressing Bias in AI Algorithms and Training Data
Bias isn’t some niche issue—it’s a real problem that can lead to missed diagnoses, wrong treatments, and unequal care. AI systems only know what we train them on, so if the data is skewed, the outcomes can be, too. Here’s how bias creeps in and what can be done about it:
- Not all populations are represented equally in health data (some have tons of data, others almost none), so AI can overlook certain groups.
- If old data has historic inequalities, the AI will pick up on those patterns and repeat them.
- Labels and annotations are sometimes inconsistent or plain wrong, which messes up the algorithm’s learning.
To chip away at these problems, hospitals and developers should:
- Collect and use data from people of all backgrounds, ages, and regions.
- Regularly test AI tools to see if their results are fair for everyone.
- Ask outside experts to review systems before rolling them out.
Ensuring Data Privacy and Security in Healthcare
Patients have every right to worry about where their data goes. Health information is personal, and leaks or hacks can cause real harm. Laws like HIPAA (in the US) and GDPR (in the EU) set standards, but here’s what good data protection in AI really looks like:
- Encrypt every bit of personal information—no exceptions.
- Limit who has access and track every login or data transfer.
- Require patient consent before using or sharing any health data.
- Monitor systems for unauthorized access or weird activity.
Sample Data Security Checklist
| Security Measure | Requirement |
|---|---|
| Data encryption | Always (at rest & transit) |
| Access control | Role-based, logged |
| Consent | Explicit, documented |
| Breach monitoring | 24/7 with alerts |
| Regular audits | Quarterly minimum |
Establishing Standards and Regulatory Oversight
It’s one thing to have cool new tools and another to actually use them safely. Standards and oversight keep everyone on the same page, especially since AI is moving fast. So what should be in place?
- Clear guidelines for how AI results are reviewed or double-checked by humans.
- Requirements for transparency—patients and doctors should know how decisions were made.
- National and international regulators that keep up with the tech and update the rules.
A few steps healthcare organizations can take:
- Work with medical boards, tech experts, and patient groups to write clear policies.
- Set up a system for patients and staff to report problems or weird outcomes.
- Regularly review AI performance and report findings publicly.
In short, making AI in diagnostics ethical and equitable is not optional—it’s the only way to build real trust and improve care for everyone. It’s not a one-and-done thing either; these issues need attention all the time, even as technology changes.
Building Trust and Acceptance Among Healthcare Stakeholders
Patient Perspectives on AI-Driven Diagnostics
Trust is at the center of any healthcare experience, so it’s no surprise that AI in diagnostics raises a lot of questions for patients. Many people worry about accuracy, privacy, and whether a computer can truly understand their unique cases. Surveys in the US show mixed feelings: around 60% of folks feel uneasy about doctors depending on AI, but up to 80% are open to using AI-based tools if they know these systems are supporting their care, not running the show.
Some reasons patients feel more comfortable with AI in diagnostics:
- When a human doctor is still involved in decisions, not just a machine
- Clear explanations about how their data will be used and stored
- Proof that AI tools are tested, safe, and regularly updated
So, honestly, trust grows when patients see transparency and continued involvement from actual people.
Collaborating with Healthcare Professionals for Adoption
Doctors, nurses, and tech staff have the most day-to-day contact with AI. Their buy-in can make or break whether these systems actually get used. Genuine acceptance really takes teamwork across professions. Here’s what helps get everyone on board:
- Including a mix of clinical staff, data scientists, and IT experts in planning and testing new tools
- Ongoing training so teams understand how AI works and what it can (and can’t) do
- Feedback loops that let staff flag problems or suggest improvements
- Respecting clinical judgment—AI should inform, not override, expert opinion
When everyone’s part of the process, there’s more trust in the technology and fewer surprises.
Communication and Transparency in AI Decision-Making
AI systems don’t always give clear reasons for their decisions. That lack of explanation drives skepticism for patients and confusion for clinicians. To improve things, healthcare organizations can:
- Use plain language to explain how an AI comes to its conclusions
- Offer summaries of which data and criteria were most important for a specific result
- Document limitations or areas where the system still needs improvement
| Stakeholder | Top Concern | Needed for Trust |
|---|---|---|
| Patients | Data security, errors | Transparent info, user control |
| Clinicians | Workflow fit, liability | Training, clear outputs |
| Admins | Cost, regulation | ROI clarity, compliance |
Transparency—about strengths, weaknesses, and updates—makes it easier for everyone to feel confident using AI in diagnostic care.
Overcoming Challenges in Adoption of AI in Medical Diagnostics

Implementing AI in healthcare sounds promising, but honestly, it faces a stack of hurdles. Some of these problems are interconnected, and addressing one doesn’t automatically solve the others. Let’s break it down.
Improving Data Quality and Accessibility
One of the main headaches in AI for diagnostics is data—too often, medical records are incomplete, scattered across different clinics, or stored in old software that barely works. To fix this, hospitals and developers are trying things like:
- Setting basic standards for how medical info is recorded
- Encouraging collaboration between clinics and labs to share cleaned-up, labeled data
- Training staff to label and enter data properly from the start
Here’s a quick table with typical data issues versus what’s needed for solid AI training:
| Challenge | Ideal for AI |
|---|---|
| Missing values | Complete records |
| Non-standard formats | Unified formats |
| Unlabeled data | Well-labeled |
Navigating Technical and Infrastructure Barriers
Not every clinic has the juice—tech-wise or money-wise—to run modern AI. Some places have ultra-fast servers; others are stuck with ancient computers. Moving to digital records is expensive, too. Common roadblocks include:
- Outdated hardware and poor internet
- Limited IT staff for set-up and troubleshooting
- Difficulty merging AI tools into existing medical software
A few ways people are tackling it: using cloud services, open-source AI platforms, and working with regional healthcare networks to pool resources.
Scaling AI Solutions Across Healthcare Systems
Once an AI algorithm works at one hospital, rolling it out everywhere is a different beast. What works in a big-city hospital may flop in a rural clinic. Problems pop up like:
- Local differences in how tests are done or data is stored
- Resistance from staff who are unsure about new tech
- Adjusting AI systems to legal rules in each state or country
Scaling up means constant updates, training sessions for staff, and often a mix of manual checks plus AI—especially in the beginning. No single fix will work everywhere, so it’s a bit of a trial-and-error process.
Putting all these pieces together takes time, patience, and a willingness from everyone—from hospital CEOs to nurses on night shifts—to work through the bumps. But even with all these headaches, most experts agree it’s worth the trouble, so that one day, good diagnostics won’t depend on your zip code.
Conclusion
So, looking at everything, it’s clear that AI is starting to change how we approach medical diagnostics. It’s not just about faster test results or fancy machines—AI is helping doctors spot things they might have missed and make decisions with more confidence. Sure, there are still some bumps in the road, like making sure the data is good and keeping patient info safe. But the progress so far is pretty exciting. As these tools get better and more common, patients could see quicker answers and better care. It’s not magic, but it’s a big step forward. The future of healthcare might not look exactly like science fiction, but with AI in the mix, it’s definitely heading somewhere new.