It feels like everywhere you look these days, AI is being talked about, and healthcare is no exception. We’re seeing a lot of discussion about how artificial intelligence could really change how doctors diagnose illnesses and how hospitals run. It’s not just about fancy new gadgets; it’s about making things more accurate, faster, and even more personal for patients. This article takes a look at what these ai medical diagnosis tool advancements might mean for everyone involved in healthcare.
Key Takeaways
- AI is getting really good at looking at medical images, like X-rays and scans, to spot problems that might be hard for the human eye to catch. This can help find diseases earlier.
- These AI tools can help speed things up in hospitals. Think about getting patients seen faster in the emergency room or automating some of the paperwork that takes up so much time.
- AI can help doctors figure out the best treatment for each person based on their specific health information. It’s like getting a treatment plan made just for you.
- Some specific areas of medicine, like heart health and brain scans, are already seeing big changes thanks to AI helping with diagnosis.
- There are still some hurdles to clear before AI is used everywhere, like making sure patient information stays private, dealing with the costs, and training people to use the new systems.
Enhancing Diagnostic Accuracy with AI
It’s pretty amazing how AI is starting to change how doctors figure out what’s wrong with people. Think about it, instead of just relying on a doctor’s eyes and experience, we now have tools that can look at scans and data with incredible detail. These AI systems are getting really good at spotting things that might be missed by the human eye, especially in those early stages of a disease.
When it comes to medical images like X-rays, CT scans, and MRIs, AI is making a big difference. These programs can be trained on thousands, even millions, of images. This allows them to learn what normal looks like and what signs of illness might be hiding. For example, studies have shown AI can be better than humans at finding certain types of cancer on mammograms or spotting signs of eye diseases from retinal scans. It’s not about replacing doctors, but giving them a super-powered assistant.
Here’s a look at how AI is helping:
- Image Analysis: AI can analyze medical images with a level of detail that’s hard for humans to match consistently. It can identify subtle anomalies in X-rays, MRIs, and other scans, helping to catch diseases earlier.
- Early Detection: By processing large amounts of patient data, including genetic information and lifestyle factors, AI can help identify individuals at higher risk for certain conditions before symptoms even appear.
- Reducing Mistakes: Human error is a factor in any field, and medicine is no different. AI can act as a second check, reducing the chance of misdiagnosis due to fatigue or oversight.
We’re seeing some really impressive numbers too. In one study looking at mammograms for breast cancer, AI systems showed a significant reduction in both false positives and false negatives compared to traditional methods. Another study found AI was more sensitive in detecting breast cancer masses than human radiologists. It’s clear that AI is not just a futuristic idea; it’s actively improving diagnostic accuracy right now.
Streamlining Healthcare Operations
Healthcare systems are always looking for ways to work smarter, not just harder. AI is stepping in to help make things run more smoothly behind the scenes, which ultimately benefits everyone. Think about how much time is spent on tasks that don’t directly involve patient care. AI can really cut down on that.
AI for Efficient Patient Triage
When patients arrive at a clinic or hospital, figuring out who needs to be seen first can be a complex process. AI can analyze a patient’s reported symptoms and vital signs to help prioritize care. This means that those with more urgent conditions can be seen quicker, reducing the risk of their health worsening while they wait. It’s like having an extra set of eyes that can process information incredibly fast. This system can also help direct patients to the right department from the start, cutting down on unnecessary transfers and delays. For example, an AI tool could flag a patient presenting with chest pain as high priority, ensuring they are seen by a cardiologist without delay.
Automating Administrative Tasks
Let’s be honest, paperwork and administrative duties can bog down any healthcare professional. AI can take over many of these repetitive tasks. This includes things like scheduling appointments, managing patient records, processing insurance claims, and even transcribing doctor’s notes. By automating these processes, healthcare staff can dedicate more time to direct patient interaction and complex medical decision-making. Imagine a world where your doctor spends less time typing and more time talking with you about your health. This shift can lead to a more positive patient experience and better job satisfaction for medical staff. Some systems are already using AI to sort and file patient documents automatically, saving hours of manual labor each week.
Reducing Outpatient Waiting Times
Waiting rooms can be a source of frustration for patients. AI can help optimize clinic schedules and patient flow to minimize these wait times. By predicting patient volume and appointment durations, AI can help manage resources more effectively. This might involve adjusting staffing levels or allocating examination rooms more efficiently. The goal is to create a more predictable and less stressful experience for patients seeking outpatient care. For instance, AI can analyze historical data to predict peak times and suggest adjustments to appointment slots to spread out patient arrivals. This technology can also help manage the flow of patients between different departments, such as from imaging to consultation rooms, making the entire process more efficient. This approach not only improves patient satisfaction but also allows clinics to see more patients, increasing overall access to care. The integration of AI into scheduling and patient flow management is a key step towards a more responsive healthcare system, and you can see how this is changing the landscape of medical services.
Personalizing Patient Care
It’s pretty amazing how AI is starting to help doctors figure out the best way to treat each person. Instead of a one-size-fits-all approach, we’re moving towards care that’s really made for you. This means looking at your specific health data, your genes, and even how you live your life to come up with a plan.
AI-Driven Treatment Recommendations
AI can sift through tons of medical research and patient data way faster than any human could. It spots patterns that might suggest a certain treatment will work better for someone with your particular condition and genetic makeup. Think of it like having a super-smart assistant for your doctor, helping them pick the most effective drugs or therapies. This is a big step from just following general guidelines; it’s about getting the right treatment to the right person at the right time. For example, in cancer care, AI can analyze genetic profiles of tumors to suggest targeted therapies, which often have better results and fewer side effects. It’s all about making medicine more precise.
Tailored Health Advice for Patients
Beyond just treatments, AI can also help give you advice that’s specific to your life. Imagine an app that doesn’t just tell you to eat healthy, but suggests meals based on your dietary needs, activity levels, and even what’s in season. Wearable devices are also playing a role here, collecting real-time data that can inform personalized health tips. This kind of tailored advice can make it easier to stick to healthy habits and manage chronic conditions. It’s like having a personal health coach available 24/7, helping you make better choices every day. This can be especially helpful for managing conditions like diabetes or heart disease, where daily habits make a big difference. You can find more about how these devices work on wearable technology.
Predictive Analytics for Health Management
This is where AI really gets interesting. By looking at your past health records and comparing them with data from millions of other people, AI can start to predict what health issues you might face down the road. It can flag you as being at higher risk for certain diseases, like heart problems or diabetes, long before you show any symptoms. This gives doctors a chance to intervene early, perhaps with lifestyle changes or preventative treatments, to stop those problems from developing in the first place. It’s a shift from treating sickness to actively preventing it, which is a much better way to stay healthy. This proactive approach could really change how we manage our long-term well-being.
Advancements in Specialized Fields
AI isn’t just a general tool; it’s really starting to make waves in specific areas of medicine. Think about it – different medical fields have unique data and challenges, and AI is proving to be pretty good at tackling those.
AI in Cardiology Diagnostics
When it comes to the heart, AI is showing some serious promise. It can look at electrocardiograms (ECGs) and other heart data, spotting patterns that might be too subtle for the human eye. This means potentially catching heart conditions earlier. For instance, AI models are being trained to identify arrhythmias or signs of heart disease from ECG readings with impressive accuracy. Some studies have shown AI algorithms can detect certain heart conditions with accuracy rates comparable to, or even exceeding, experienced cardiologists. This could lead to quicker diagnoses and better treatment plans for patients.
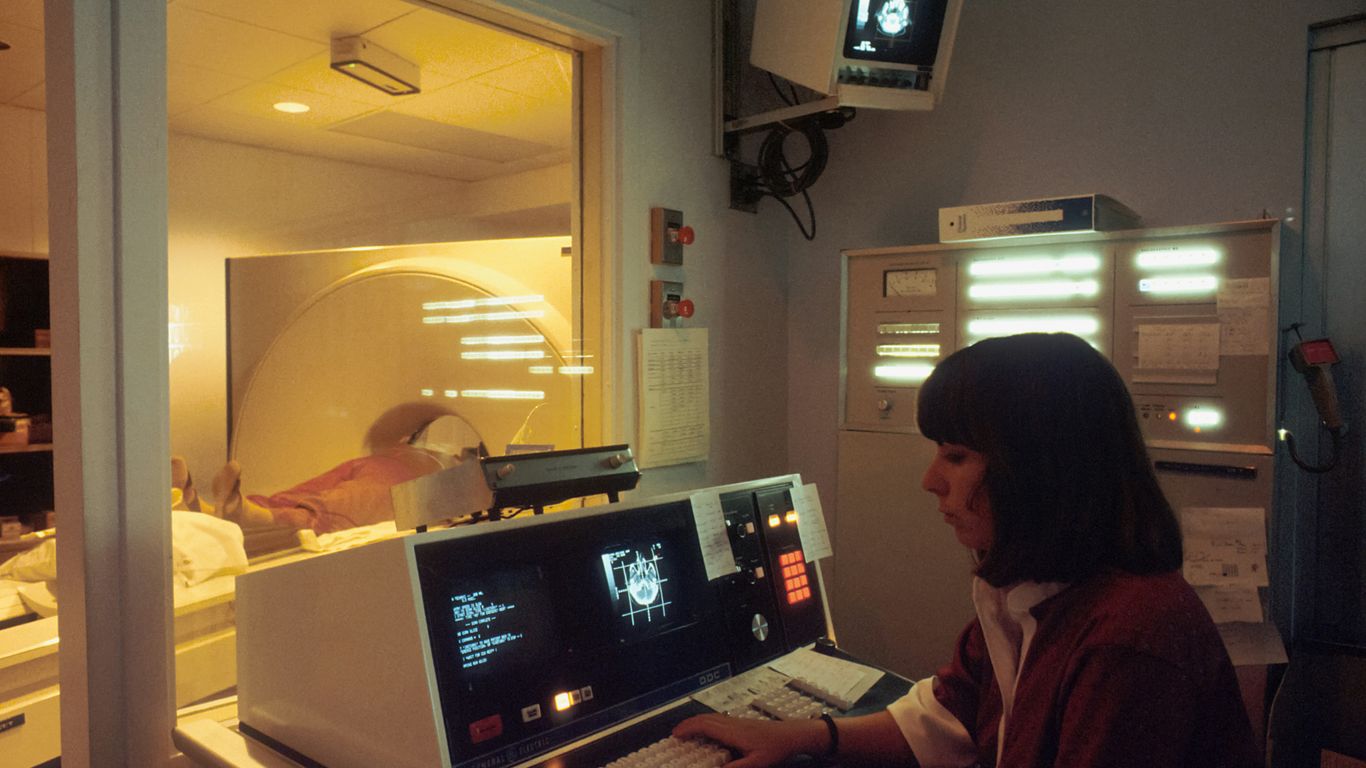
AI’s Impact on Radiology Workflows
Radiology is another area where AI is making a big difference. AI can help radiologists by sifting through a huge number of medical images, like X-rays, CT scans, and MRIs. It can flag suspicious areas that might need closer inspection, essentially acting as a second pair of eyes. This doesn’t replace the radiologist, but it can speed up the process and help them focus on the most critical cases. Imagine an AI system that can quickly identify potential fractures or tumors in scans, allowing the radiologist to spend more time on complex diagnoses. This efficiency boost is really important given the increasing volume of imaging studies being done.
AI in Neurological Assessments
For conditions affecting the brain and nervous system, AI is also proving useful. Analyzing brain scans, like MRIs or EEGs, can be complex. AI can help by identifying subtle changes associated with neurological disorders such as Alzheimer’s disease, Parkinson’s, or even early signs of stroke. It can process large datasets of brain imaging and patient data to find correlations that might not be obvious. For example, AI is being explored to help predict the progression of neurological diseases or to assist in the interpretation of complex EEG patterns, which could lead to more personalized treatment strategies for patients with neurological conditions.
Addressing Challenges in AI Adoption
So, while AI in medicine sounds pretty amazing, getting it into hospitals and clinics isn’t exactly a walk in the park. There are a bunch of hurdles we need to jump over first. Think about it: these systems need tons of data to learn, and getting that data in a clean, usable format is a huge job. Plus, making sure the AI plays nice with all the existing computer systems in a hospital? That’s another headache. And let’s not forget the price tag – these tools can be really expensive to buy and set up. On top of that, doctors and nurses need to know how to use them, which means training, and that takes time and resources. It’s not just about the tech, though. We also have to figure out who’s responsible if an AI makes a mistake, and how to keep all that sensitive patient information safe from hackers. It’s a lot to sort out before AI becomes a regular part of how we do healthcare.
Navigating Ethical Considerations
One of the big worries with AI in medicine is making sure it’s fair. AI learns from the data it’s given, and if that data has biases – maybe it mostly comes from one group of people – the AI can end up making unfair recommendations for others. This could lead to some patients getting less than ideal care just because the AI wasn’t trained on data that represented them well. We also need to think about transparency. If an AI suggests a certain treatment, doctors and patients should understand why. The ‘black box’ problem, where we don’t know how the AI reached its conclusion, is a real concern. It’s like getting advice from someone you can’t question. Building trust means we need AI systems that can explain their reasoning, especially when patient lives are on the line.
Ensuring Data Privacy and Security
Healthcare data is incredibly personal, and keeping it safe is non-negotiable. AI systems often need access to vast amounts of patient information to work effectively. This creates a big target for cyberattacks. We have to build really strong security measures to protect this data from being stolen or misused. Think of it like a digital vault. Not only do we need to protect against outside threats, but we also need to make sure that only authorized people and systems can access specific data. This involves careful planning of who gets to see what and how that information is stored and transmitted. It’s a constant cat-and-mouse game with security, and the stakes are incredibly high.
Overcoming Cost Barriers and Training Needs
Let’s be real, implementing new technology in healthcare is expensive. AI diagnostic tools are no different. Hospitals and clinics need to invest a lot of money upfront for the software, the hardware, and then the ongoing maintenance. For smaller practices or hospitals in less wealthy areas, this cost can be a major roadblock. Beyond the financial side, there’s the human element. Doctors, nurses, and technicians need to be trained on how to use these new AI tools correctly. This isn’t just a quick tutorial; it often requires dedicated training programs to make sure everyone is comfortable and competent. Without proper training, the tools might not be used to their full potential, or worse, could be used incorrectly, leading to errors. It’s a two-part challenge: making the technology affordable and making sure the people using it are well-prepared.
The Future of AI Medical Diagnosis Tools
So, where are we headed with all this AI in medicine stuff? It’s pretty exciting, honestly. We’re not just talking about making current tools a bit better; we’re looking at a whole new way of doing things.
Integrating AI into Clinical Practice
Getting AI tools into the everyday workflow of doctors and nurses is the next big step. It’s not as simple as just installing software, though. Think about it: doctors are already swamped. We need these AI systems to be easy to use, to fit right in, and to actually save them time, not create more work. It’s about making AI a helpful assistant, not another complicated gadget.
- Training and Education: Healthcare workers will need to learn how to use these new tools effectively. This means updated training programs and ongoing support.
- Workflow Redesign: Hospitals and clinics will have to rethink how they operate to make the best use of AI.
- Interoperability: AI systems need to talk to existing hospital systems, like electronic health records, without a hitch.
Building Trust in AI Healthcare Solutions
People are naturally a bit wary of new technology, especially when it comes to their health. For AI to really take off, patients and doctors alike need to trust it. This means being open about how the AI works, what its limitations are, and what happens if something goes wrong. Transparency is key here.
- Explainable AI (XAI): We need AI that can explain its reasoning, so doctors can understand why a diagnosis was suggested.
- Performance Validation: Rigorous testing and real-world studies are vital to prove these tools are safe and effective.
- Clear Accountability: Who’s responsible if an AI makes a mistake? Establishing clear lines of responsibility is a must.
The Evolving Landscape of AI in Medicine
This field is moving at lightning speed. What seems cutting-edge today might be standard practice tomorrow. We’re seeing AI get better at spotting diseases earlier, personalizing treatments, and even helping with the administrative side of healthcare, which is a huge win for everyone.
- Quantum Machine Learning: This advanced form of AI could lead to even more powerful diagnostic tools and help discover new medicines.
- AI in Pathology: AI will likely take over many of the repetitive tasks in analyzing tissue samples, freeing up pathologists to focus on complex cases and patient outcomes.
- Predictive Health: AI will get even better at forecasting health risks, allowing for proactive interventions before problems become serious. The ultimate goal is to shift healthcare from being reactive to being truly proactive.
Looking Ahead
So, where does all this leave us? It’s pretty clear that AI is set to change how we do healthcare, especially when it comes to figuring out what’s wrong with people. From spotting cancer early to making sure patients get the right treatment for them, AI tools are showing they can really help. They can speed things up, catch things humans might miss, and even help doctors make better choices. But, it’s not all smooth sailing. We still need to sort out privacy issues, make sure these tools are used fairly, and figure out who’s in charge when AI is involved in patient care. Building trust is a big part of this, and that means being open about how these systems work. If we can get past these hurdles, AI could really make healthcare better for everyone, leading to healthier lives and a system that works more smoothly for both patients and the people who care for them. It’s a big step, but one that could lead to a healthier future.