The Pioneering Era of Surgical Robotics
Early Concepts and Prototypes in Robotic Surgery
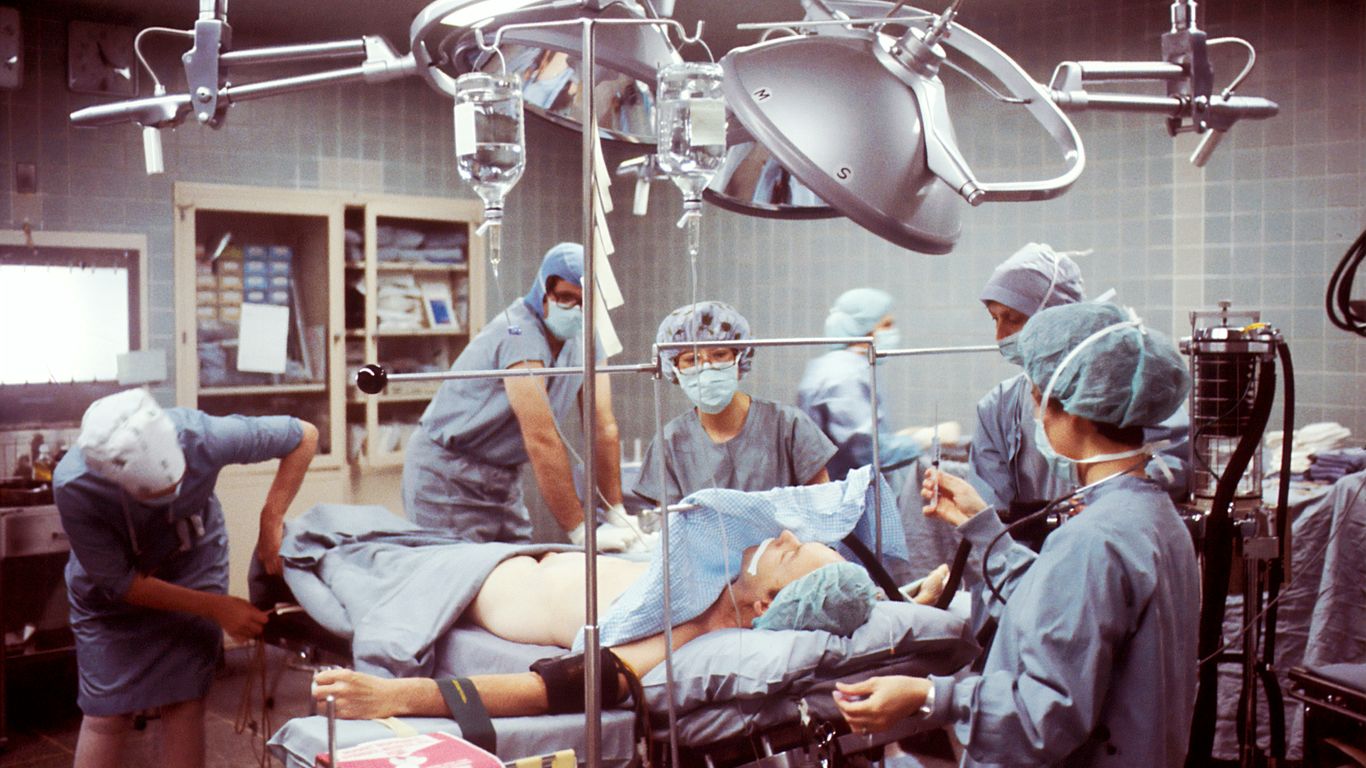
It’s wild to think that the story of surgical robots doesn’t just start with high-tech companies. Instead, it actually goes back to some pretty unexpected roots: science fiction dreams, military needs, and even the early days of the space race. In the 1970s, projects funded by NASA and DARPA started pushing for safer methods to perform surgery remotely—imagine trying to operate on an astronaut in orbit or a soldier in a warzone without ever being in the room. Their goal? Create machines that could do the heavy lifting—and delicate trimming—when humans simply couldn’t get there in person.
Some major early milestones:
- The PUMA 560 robot performed a neurosurgical biopsy on a real patient in 1985—no small feat back then.
- Only a few years later, the ProBot, developed at Imperial College London, tackled prostate surgery with its compact, smart design and speedy rotating blade.
- The 1990s saw IBM and other innovators release systems like ROBODOC®, capable of prepping bones for hip replacements.
Key Projects by NASA and DARPA
It’s honestly amazing how space exploration ended up shaping surgical technology back on Earth. NASA and other agencies didn’t just want better rockets—they needed solutions for medical emergencies in space. There was real pressure to invent telemanipulation, where a doctor’s hands could control robotic arms from miles (or even hundreds of miles) away.
Some key efforts included:
- Developing virtual reality displays so surgeons could see a 3D view as they operated
- Focusing on remote manipulation for safer surgeries in dangerous or hard-to-access spots
- Bringing the operating room as close as possible to the patient, whether that was a battlefield, space station, or disaster site
Reading about these early breakthroughs, it’s clear that military and space challenges shaped the way human-like robots enhance safety, as well as medical tech overall.
The Advent of Telepresence in Surgery
Telepresence sounds like something from a sci-fi movie, but in surgery, it means using technology to let doctors "be" in two places at once. The Automated Endoscope System for Optimal Positioning (AESOP), built by Computer Motion, took a major step forward with FDA approval in 1994. This allowed surgeons to control a camera with their voice, making procedures smoother:
Key points about early telepresence systems:
- Surgeons could direct endoscopes using simple voice commands
- Later systems, like ZEUS, let doctors perform entire procedures from a remote console
- These robots kicked off a new era, where precision and distance didn’t have to get in the way of good medicine
Most surgeons probably didn’t think, back in the 1980s, that robots would ever help them out in the OR. Yet, by the end of the decade, robotics was on its way to becoming a standard part of surgery—setting the stage for bigger names and bigger leaps, just around the corner.
When Was the Da Vinci Robot Invented and Its Initial Impact
Development Timeline and First Human Use in 1998
Frankly, robotic surgery wasn’t really on the medical radar in the early ’90s. But things ramped up quickly. By 1995, Intuitive Surgical was founded, and it set out to create something that honestly sounded like science fiction at the time: a robot that lets humans do surgery without even touching the patient directly. The very first use of the da Vinci system on a human happened in 1998. It was tested out in Europe, starting with things like heart valve repairs and cholecystectomies (removing gallbladders). Back then, even seasoned surgeons found the whole thing a bit surreal. But the difference was clear—the incisions were smaller, and surgeries took less time. Everyone in the medical field was buzzing.
Here’s a quick timeline of its early days:
| Year | Milestone |
|---|---|
| 1995 | Intuitive Surgical founded |
| 1998 | First human da Vinci procedure |
| 1998 | First commercial sale (Germany) |
FDA Approval and Commercial Launch in 2000
After those first successful procedures, the team at Intuitive started working with US regulators. Getting FDA approval isn’t easy—especially for something so new. There were questions about safety, how reliable the robot was, and whether it could actually help surgeons do a better job. After lots of paperwork (and nerves), the da Vinci Surgical System received FDA approval for general laparoscopic procedures in 2000. This made it the first operative surgical robot cleared for widespread use in the United States. Hospitals were initially cautious because the tech was new and expensive, but there was no going back—robotic surgery had officially arrived.
Milestone Surgeries and Medical Advancements
Once it got FDA approval, things moved fast. Surgeons started using the da Vinci for all sorts of procedures. These were some of the big early milestones:
- First cardiac valve repairs and coronary bypasses without cracking open the chest—huge for patient recovery.
- Laparoscopic prostate removals that left patients with less pain and quicker returns to normal life.
- Complex gynecologic surgeries performed with much tinier scars than before.
There was a real snowball effect. By reducing hand tremors and scaling down fine movements, the da Vinci allowed people to:
- Operate on tough-to-reach places without big cuts.
- Shorten hospital stays for most patients.
- Start thinking about surgery in a way that just wasn’t possible before 1998.
Looking back, it’s clear those first years changed how everyone—from patients to surgeons—thought about what was possible in the operating room.
Key Innovations Behind the Da Vinci Surgical System
The Da Vinci Surgical System didn’t just pop out of nowhere—it brought some big changes that made surgeons and hospitals rethink what was possible in the operating room. Let me break down the core features that set it apart.
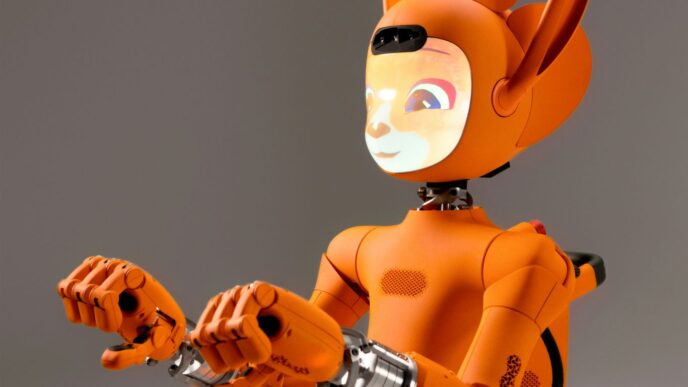
Design Features and Technological Components
- The Da Vinci isn’t one single boxy robot. It’s a setup with three separate parts:
- The surgeon console, where the doctor sits and controls everything while looking into a 3D viewer.
- The patient cart, which holds the multi-jointed robotic arms right at the operating table.
- The vision cart, which connects it all and manages the camera’s high-definition, real-time feed.
- Each arm is super flexible, a bit like a human wrist, so the movements can feel natural but way more steady and tight.
- The tools can be swapped out, so you can attach scissors, forceps, or even advanced sealers and staplers.
What stands out is how these design choices allow a human surgeon to become hyper-precise while sitting down, with every movement translated directly to the working arms and instruments.
Console, Arms, and 3D Vision Integration
- The main console comes with a stereoscopic display, so surgeons see a true three-dimensional, magnified image of the patient’s insides.
- Two master handles let the surgeon manipulate tools as if using their own hands—but calibrated and miniaturized at the surgery site.
- The original three-arm setup had a camera arm and two instrument arms, but the newer four-arm design made it easier to do complex steps alone, cutting down on the need for a surgical assistant.
Here’s a quick comparison of some models:
| System | Number of Arms | 3D Camera | Notable Upgrades |
|---|---|---|---|
| Standard | 3 | Yes | Basic HD, manual setup |
| S (2006) | 4 | Yes, HD | Touchscreen, easier set-up |
| Si (2009) | 4 | Yes, HD/3D | Dual console, better imaging |
| Xi (2014) | 4 | Yes, advanced | Enhanced flexibility, stapling |
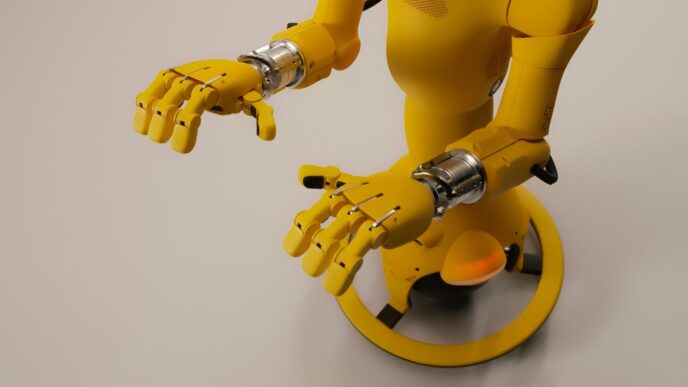
Elimination of Surgeon Hand Tremors
- One of the big headaches in fine surgery is hand shakiness—even the best surgeons can’t stay perfectly steady after hours.
- The Da Vinci filters out any little shakes in real time, so the robot only carries out intentional movements.
- There’s also movement scaling: if a surgeon moves a handle one inch, the robot can be set to move one-fifth of an inch. That’s a big deal when working near nerves or blood vessels.
So, to sum it up:
- The robot lets surgeons do things steadily that they could never do by hand.
- 3D vision makes doctors feel like they’re literally inside the patient.
- Modular arms and smart instruments turn the robot into a do-it-all surgical partner.
Modern surgery keeps moving forward, and the Da Vinci’s core system is still one of the main reasons why.
Comparing Da Vinci to Its Predecessors and Contemporaries

ZEUS Robotic System vs. Da Vinci
You can’t really talk about the da Vinci system without looking at the ZEUS robotic system first. ZEUS came out in the mid-1990s, made by Computer Motion, and it was used mainly for laparoscopic and heart surgeries. ZEUS had two robotic arms and relied on AESOP, a separate voice-controlled endoscopic arm. Surgeons controlled everything from a distance using a console, but the view was usually just basic 2D, sometimes with clunky polarized 3D effects.
Da Vinci, which first hit operating rooms in the late 1990s, changed a lot about what robotic surgery could do. It offered:
- A 3D high-definition vision system that really let surgeons see depth and detail.
- Three (and later four) modular robotic arms, all on one cart—ZEUS made you mount each arm separately.
- Controls that filtered out hand tremors and could even downscale large movements, which helped with delicate work.
- Instruments that mimicked the natural movement of the human wrist.
Here’s a table that breaks down some main differences:
| Feature/Aspect | ZEUS | Da Vinci |
|---|---|---|
| Release Year | 1998 (FDA: 2001) | 1998 (FDA: 2000) |
| Arms | 2 (+ AESOP) | 3–4, all on integrated cart |
| Vision | 2D/Polarized 3D | True HD 3D |
| Clinical Use | Discontinued (2003), Heart/Lap | Widely adopted, multi-specialty |
| Cost | Less expensive | Higher price, more features |
| Company | Computer Motion | Intuitive Surgical |
After Intuitive Surgical and Computer Motion merged in 2003, ZEUS was discontinued and da Vinci became the dominant player, shaping how hospitals approached robotic surgery.
Lessons Learned from Early Robotic Platforms
Looking back at the evolution from ZEUS and other early systems to da Vinci, a few things stand out:
- Integrated systems are much easier for surgical teams to use than modular, table-mounted arms.
- 3D vision provides a genuine advantage in precision compared to standard 2D screens.
- Users (surgeons) want intuitive, ergonomic controls that cut down fatigue and allow for fine-tuned movements.
- Scaling and filtering surgeon input (for things like hand shake) makes complex tasks much safer.
Robotic surgery had to meet practical demands in the real world, and not just look slick in the lab. Simplifying setup was a big deal for operating room staff, and giving surgeons a more immersive, less tiring experience proved to be a key factor in adoption.
Influence of Previous Innovations on Da Vinci
Da Vinci didn’t come out of nowhere—the people behind it took direct inspiration from earlier efforts:
- Telepresence surgery ideas pushed by NASA and the military showed surgeons could operate at a distance—this technology was adapted for civilian hospitals.
- Wristed instruments and endoscopic cameras already existed but had clear limits; da Vinci built on them, making more advanced versions that could move more naturally.
- Feedback from surgeons who used ZEUS and other early robots helped shape da Vinci’s hands-on features, like motion scaling and the improved visualization.
In short, da Vinci stands on the shoulders of earlier robots, blending lots of “what worked” from a bunch of earlier systems, and fixing the things that annoyed real surgeons. The end result? A system that many hospitals now consider standard for minimally invasive surgical work, while the older names like ZEUS have faded away.
Ongoing Evolution and Generational Advancements
The da Vinci Surgical System has seen a steady pace of upgrades over the past two decades, each generation building on lessons from the last. It’s sort of wild to think how far these robots have come since their early days, and honestly, the tech keeps getting smarter and more adaptable every couple years.
The S, Si, and Xi Da Vinci Systems
Let’s break down the main da Vinci generations that changed the operating room scene:
- Da Vinci S (2006): This version introduced better ergonomics for surgeons and improved vision with advanced 3D capabilities. It was more reliable but still bulky and not super easy to set up.
- Da Vinci Si: The Si system gave surgeons dual-console setups (think two surgeons at the same system), and it added high-def, 3D imaging. Still, it had large, parallel arms that made arm collisions a problem and multiquadrant surgery pretty clunky.
- Da Vinci Xi (2014): With this model, Intuitive Surgical made a serious leap. The Xi platform redesigned the cart and arm setup so the system could move between quadrants during one procedure without a lengthy undocking/redocking process. The arms were streamlined, ports were smaller, and overall, it became much more flexible for surgeons handling complex or multi-site cases (rapid progress in AI).
Here’s a simple table to show how each version stacks up:
| Generation | Key Upgrades | Release Year |
|---|---|---|
| S | Improved 3D vision, better ergonomics | 2006 |
| Si | Dual-console, HD vision, more options | Late 2000s |
| Xi | Flexible arms, smaller ports, smarter design | 2014 |
Enhanced Surgical Features Over Time
The da Vinci system’s tech isn’t just about fancy cameras and more arms. Each upgrade included meaningful surgical improvements, like:
- More robust instrument control for fine work, such as vascular sealing and robotic stapling.
- Real-time imaging with 3D high-def visualization for precision targeting.
- Upgraded surgical accessory kits, including single-port and Endowrist tools that improve range of motion and tactile feedback.
- Faster setup, easier docking, and reduced arm collisions, which used to be a headache.
Even weirdly specific stuff—like smarter staplers and more flexible suction tools—got built in. The newer Xi and SP (Single Port) platforms made big progress for crowded anatomical spots and complicated procedures.
Improvements in Surgeon Training and Capabilities
It’s not just the hardware that moved forward. The way surgeons learn and work with these robots has totally changed. Training is a much bigger deal now, and the platforms help surgeons improve their skills over time:
- Structured simulation modules for new and experienced surgeons.
- Dual console feature allows live mentoring, so surgeons can trade off seamlessly during a real case.
- Regular software upgrades introduce smoother workflow, better camera control, and more personalized tactile feedback.
The result is safer surgeries, shorter learning curves, and a wider range of doctors who can take on minimally invasive approaches.
And looking forward, it’s clear da Vinci’s evolution is part of a much bigger race in medical robotics—especially as AI and integrated smart tools become common throughout healthcare.
The Da Vinci Robot’s Influence on Modern Medicine
Impact on Patient Outcomes and Recovery
Robotic-assisted surgery with the Da Vinci system has really changed the way we think about patient recovery. Instead of huge incisions, most surgeries now can be done through tiny cuts—less pain and smaller scars. Most people notice they can get back to their normal routines much faster than with old-school surgery. Fewer complications and lower infection risk have been big selling points for both doctors and patients. Here’s how outcomes typically compare:
| Surgery Type | Typical Recovery (Traditional) | Typical Recovery (Da Vinci) | Blood Loss | Hospital Stay |
|---|---|---|---|---|
| Prostatectomy | 4-6 weeks | 1-2 weeks | Less | Shorter |
| Hysterectomy | 4-6 weeks | 2 weeks | Less | Shorter |
| Mitral Valve Repair | 6-8 weeks | 3-4 weeks | Less | Shorter |
A lot of people feel more comfortable choosing surgery now since they know the healing process won’t be as rough. Plus, there’s less need for heavy pain meds.
Expansion of Minimally Invasive Procedures
Back when Da Vinci first arrived, robotic surgery was pretty much just for urology procedures, but that changed pretty quickly. Now it’s common in:
- Gynecology (hysterectomies, endometriosis)
- General surgery (hernia repairs, gallbladders)
- Heart surgery (mitral valve repairs)
- Colorectal and thoracic surgeries
What’s wild is how some operations that used to be considered too complicated for keyhole surgery are routine now with the robot. Surgeons feel more confident working near delicate nerves and vessels, so they can try techniques that would be tricky, if not impossible, by hand.
Adoption in Hospitals Worldwide
When the Da Vinci system first launched, only a couple hospitals gave it a try. But things escalated fast once word got around about the benefits. By now, thousands of hospitals in dozens of countries use one or more Da Vinci robots. Here’s a quick breakdown of growth:
- 2000: < 10 hospitals in the US
- 2010: ~1,000 worldwide
- 2025: >6,000 worldwide (estimate)
Hospitals brag about having a Da Vinci—patients even ask about it. Not all places can afford one, but bigger hospitals usually offer robotic surgery for at least a few procedures. Da Vinci has basically set the standard for surgical robotics, influencing training and expectations everywhere.
In summary, Da Vinci’s influence isn’t just hype. It’s changed the daily reality for surgeons and patients alike, made new procedures possible, and left a mark on how hospitals market themselves and how people view surgery itself.
Visionaries and Companies Behind the Da Vinci Robot
The Role of Intuitive Surgical in Innovation
Intuitive Surgical changed the medical landscape when it brought the Da Vinci Surgical System to market. Founded in 1995, this California-based company set out to make minimally invasive surgery more accessible. Their vision: develop a robot that could give surgeons more control and better visibility, while actually making surgery easier on patients. Back in 1998, Intuitive’s first Da Vinci system was used in real human surgeries, including heart procedures that avoided the usual big chest incisions. By 2000, after gaining FDA approval, it became the first flexible, commercially available surgical robot in the US. As Intuitive grew, it kept pushing updates and new models—some highlights:
- 2000: First-generation Da Vinci launches with three arms.
- 2002: Four-arm version arrives, expanding versatility.
- 2006–2014: Major upgrades bring advanced imaging and motion control (S, Si, Xi systems).
Intuitive Surgical’s relentless drive meant hospitals around the world could offer less invasive options than ever before.
Impact of the Computer Motion Merger
In the early 2000s, Computer Motion was Intuitive’s main rival, known for its ZEUS system. Both companies wanted to lead robotic surgery—and they ended up in court over patents. By 2003, after years of legal fighting, the two companies merged. Here’s what changed post-merger:
- Intuitive absorbed ZEUS technology, stopping its further development but integrating useful ideas.
- Combined efforts accelerated improvements for the Da Vinci system.
- The merger made Intuitive the clear leader in robotic surgery—competitors faded fast.
This partnership didn’t just end a legal feud—it pulled together decades of research and propelled surgical robotics forward.
Influence of Early Robotic Surgery Researchers
A few early thinkers laid the groundwork for what became the Da Vinci. People like Phil Green, Richard Satava, and teams at the Stanford Research Institute helped shape the field. Their work for agencies like NASA and DARPA on telepresence surgery made remote, precise procedures seem possible—even on the battlefield.
Some major contributions:
- Phil Green’s telepresence concepts: set the stage for controlling surgical robots at a distance.
- Early government-funded prototypes: proved that remote surgery could work under extreme conditions.
- Emphasis on minimizing invasiveness: became the guiding idea for Intuitive’s later platforms.
Without their original research and inspiration, the Da Vinci might never have left the idea stage. For a broader sense of technology’s influence on innovation, including in other sectors, see BMW’s Vision Vehicle for another take on futuristic design.
Conclusion
So, that’s the story behind the da Vinci robot. It first showed up in the late 1990s, and by 2000, it had already made its mark in the world of surgery. Since then, it’s gone through a bunch of updates, each one making it a little better and easier for doctors to use. The da Vinci system changed how surgeries are done, making them less invasive and helping patients recover faster. Even though it’s not perfect—those robotic arms are still pretty big and sometimes get in the way—it’s clear that this technology has made a real difference in hospitals around the world. Looking back, it’s wild to think how far we’ve come from Leonardo da Vinci’s sketches to robots that can help save lives. And who knows? With the way things are going, the next big leap in surgical robots might be just around the corner.