AI in medical diagnostics is changing the way doctors spot and treat diseases. Right now, computers can look at medical images, patient histories, and even genetic data to help find problems faster and more accurately. This means doctors can make better decisions and sometimes catch illnesses before they get worse. AI is also making it easier for people in remote or underserved places to get quality care. Even though there are still some bumps in the road—like making sure patient data stays private and making sure the technology works for everyone—AI is already making a real difference in healthcare.
Key Takeaways
- AI in medical diagnostics is helping doctors find diseases earlier and more accurately.
- Medical imaging, like X-rays and MRIs, is being analyzed by AI to help spot problems that humans might miss.
- Personalized treatments are becoming more common as AI uses genetic and other patient data to recommend therapies.
- Remote healthcare is getting better with AI-powered devices and telemedicine, reaching more people in rural areas.
- There are still challenges, like keeping data safe and making sure AI is fair, but the benefits are growing every year.
Emerging Applications of AI in Medical Diagnostics
Artificial intelligence is starting to influence how doctors catch, classify, and manage diseases. It’s becoming a handy helper across hospitals and clinics—not just in futuristic labs. Here’s how it’s showing up right now:
Predictive Analytics for Early Disease Detection
AI can sift through a patient’s history, lab results, and even their heartbeat, hunting for clues that humans might miss early on. These tools spot risks way before symptoms appear, letting people get treated earlier and often with less hassle.
Main uses include:
- Scanning large datasets to predict heart attacks, strokes, and other emergencies before they happen.
- Alerting doctors to subtle changes that suggest chronic disease flare-ups or new threats.
- Using wearable tech to log changes in temperature, pulse, or blood pressure and flagging possible concerns right away.
| Disease | AI Early Detection Accuracy | Traditional Accuracy |
|---|---|---|
| Breast Cancer | 91% | 74% |
| Skin Melanoma | 87% | 81% |
| Acute Appendicitis | 84% | 76% |
While AI doesn’t replace routine checkups, it often finds things earlier, giving people a leg up on treatment.
Enhancing Disease Classification and Risk Assessment
Deciding exactly what kind of illness someone has isn’t always clear-cut. AI can compare complex lab and image results to huge libraries of past cases, helping clarify tough calls.
Some benefits:
- Quickly sorting test results to tell apart bacterial vs. viral infections, saving unnecessary antibiotics.
- Matching symptoms and genetic patterns for rare disorders, even when they baffle ordinary tests.
- Suggesting personalized risk levels based on thousands of factors, far beyond what one person can keep track of.
Key roles AI plays:
- Sorting out diseases with overlapping symptoms (like pneumonia vs. heart failure).
- Speeding up urgent triage in emergency departments by instantly highlighting dangerous patterns.
- Nudging doctors with reminders about rare but important possibilities.
Optimizing Diagnostic Workflows in Clinical Practice
Let’s face it—doctors and nurses spend too much time shuffling paperwork and searching for results. AI cuts through much of this routine by:
- Pulling together information from medical images, lab numbers, and notes for a complete view.
- Prioritizing urgent cases, like flagging abnormal scans at the top of a radiologist’s queue.
- Automatically drafting suggestion notes or reports, which doctors can double-check and sign off.
| Workflow Step | Time Without AI | Time With AI |
|---|---|---|
| Imaging Review | 15 min | 5 min |
| Lab Result Flagging | 10 min | 2 min |
| Report Generation | 12 min | 3 min |
By reducing the busywork, AI helps healthcare teams focus more on patients and less on the endless flood of data.
Bottom line: AI is popping up everywhere, from early warnings to keeping the workflow moving. The changes aren’t always flashy, but day to day, they’re making a real difference for both patients and busy care teams.
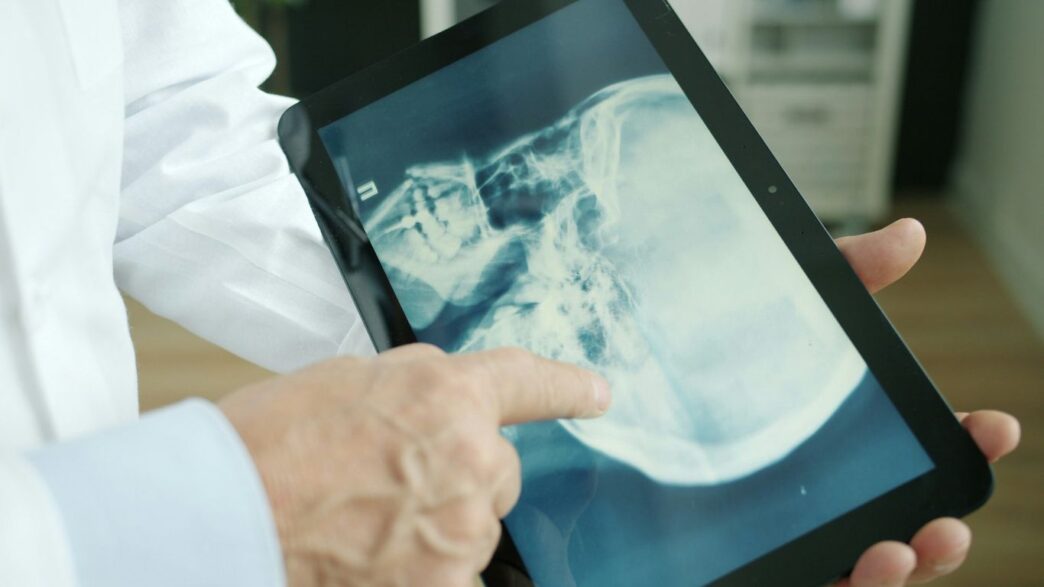
Transforming Medical Imaging with Artificial Intelligence
Artificial intelligence is changing how we look at X-rays, MRIs, CT scans, and just about any type of picture taken in a hospital or clinic. Machines are now helping doctors find signs of illness earlier and with accuracy that sometimes surprises even seasoned radiologists. Patients might not notice much on the surface—the doctor’s still there, reading results—but behind the scenes, AI is making a lot of noise. Let’s break down what’s actually happening and what it means for healthcare right now.
Improving Accuracy in Radiology and Pathology
- AI tools can spot patterns in images that are easy to miss.
- Studies show AI can reduce the number of false alarms and missed cases in cancer screening.
- Some systems even pick up on subtle features years before a human eye would.
| Use Case | AI Performance | Traditional Practice |
|---|---|---|
| Breast Cancer Mammogram Detection | 91% Sensitive | 74% Sensitive |
| Melanoma (Skin Cancer) Diagnosis | Comparable to top dermatologists | Highly variable |
| Pneumonia Detection (Chest X-ray) | 96% Sensitive | 50% Sensitive |
Sometimes, these AI systems are like a ‘second set of eyes,’ picking up things when the human brain is tired or distracted. It’s not about replacement—it’s about backup, which is handy on a tough shift.
Automating MRI and CT Scan Analysis
It’s wild how fast computers can now find problem spots in a full-body scan. They:
- Run through hundreds of slices from an MRI or CT in minutes—sometimes seconds.
- Highlight areas that need a closer look, making sure nothing gets missed.
- Provide measurements and standardize the process, shrinking the chances of errors.
Doctors still make final decisions, but they’re spending less time hunting for tiny details buried in gigabytes of data. The fatigue drops, and more patients get through the system faster.
Overcoming Challenges in Medical Imaging AI Adoption
With all these perks, you’d think hospitals would jump at using AI. In reality, it’s a slog getting everyone on board:
- Old computer systems in clinics don’t always "talk" to new AI tools.
- The "black box" problem—doctors can be hesitant to trust something they don’t quite understand.
- Regulations move slowly, and updates to medical software must be cleared for safety.
Even as machines keep getting smarter, people and hospitals need time to trust and update their routines. Change isn’t instant—sometimes it’s a grind, but that’s how progress usually works in medicine.
In short, AI isn’t just a buzzword in medical imaging anymore. It’s working its way into daily hospital life, often quietly, but with big results for accuracy and efficiency.
Personalized Medicine Through AI in Medical Diagnostics

Today, AI is changing how doctors match treatments to each person, rather than just using the same approach for everyone. This means care is based on things like your DNA, lab values, and even your daily habits, all pieced together with the help of advanced computer programs.
Utilizing Genetic and Biomarker Data for Tailored Treatments
AI programs can scan through loads of genetic and biomarker data in seconds, something that would take a person years. This makes it possible to spot who might react well to one medicine versus another, or even who might have bad side effects.
- AI can connect certain genes or proteins in your blood with likely outcomes from specific treatments
- Doctors are starting to use this data to decide which medicine and dose makes sense, even before you get sick
- Labs now use AI to read reports and flag if there’s something risky hiding in the results
Here’s a basic table showing how AI uses different data sources for treatment choices:
| Data Type | AI Role | Sample Impact |
|---|---|---|
| DNA/Genetic Tests | Predicting drug response | Choosing right cancer drug |
| Blood Biomarkers | Tracking risk | Notifying about heart risk |
| Lifestyle Data | Tweaking recommendations | Adjusting diet suggestions |
Computers can’t replace doctors, but by finding patterns in these massive data sets, they can point out options doctors sometimes miss.
Advancing Precision Oncology and Therapy Selection
Cancer care is one of the biggest places benefiting from these tools.
- Scientists feed massive gene sets and treatment records into AI to spot patterns linked with success or failure
- AI tools are also being used to guess which chemotherapy works best for a specific person, greatly improving chances
- Hospitals now use algorithms to sort cancer types by gene patterns, which helps pick targeted drugs instead of just using standard chemotherapy
Now, doctors can look at a cancer patient’s specific genetic info before choosing treatments – a huge shift from the old days of trial-and-error.
Facilitating Multidimensional Patient Profiling
It’s not just about genes—AI blends tons of other details to get the full picture of each patient.
- Medical record history, family background, food and activity habits, and even data from connected smart devices all feed into these profiles
- The AI then helps doctors predict things like disease risk, best treatments, or if a certain approach might fail
- This process is already getting simpler thanks to progress in connected technology, much like how home smart hubs are helping tie various devices together AI-powered home assistants
Personalized medicine through AI is just starting to transform regular healthcare visits from generic to specific, finally making treatment recommendations that fit each person’s unique details. This doesn’t just make care more accurate—it also sometimes prevents trouble before it even starts.
Remote Healthcare and AI-Enabled Diagnostics

Artificial intelligence is completely changing the way people get care from a distance. Everything from talking with doctors online to getting test results at home has started to feel a whole lot easier and faster. AI is helping remote care feel a bit less remote—making healthcare happen wherever you are, not just in a hospital.
Empowering Telemedicine with Real-Time Analytics
Telemedicine has been around for a while, but smart analytics powered by AI take it to another level. Instead of just a video appointment, algorithms can look at a patient’s symptoms, history, and even live data from connected devices.
Key benefits include:
- Fast, data-driven preliminary diagnosis before seeing a doctor
- Tracking small changes in symptoms over time
- Instant flags for urgent or risky situations, making it much harder for something serious to slip by
It’s getting easier for everyone—especially people who live far from clinics or struggle with mobility—to connect with doctors armed with better information than ever before.
Wearable Devices and the Internet of Medical Things
Wearables aren’t just fancy step counters anymore. They now monitor everything from heart rhythms to blood sugar, feeding real-time data right to healthcare teams or even alerting them of something abnormal. Pair that with smart AI, and suddenly devices can spot trouble before it happens.
Some real-world uses:
- Detecting irregular heartbeats before a crisis occurs
- Following chronic illnesses, like diabetes or hypertension, minute by minute
- Supporting recovery at home after surgery with continuous feedback
Check out how wearable devices use smart sensors and AI to help manage everyday health, provide feedback, and even support safety in critical situations.
| Device Type | Common Uses | AI Functionality |
|---|---|---|
| Smartwatches | Heart rate, steps, sleep tracking | Predict trends |
| Glucose Monitors | Blood sugar monitoring | Alert spikes |
| Blood Pressure | BP readings | Long-term analysis |
Bringing Quality Diagnostics to Underserved Areas
A big promise of AI-enabled diagnostics is shrinking the healthcare gap for people living in locations with few doctors, labs, or hospitals. Smart tools can:
- Analyze images like X-rays or ultrasounds on-the-spot with minimal equipment
- Allow non-specialists (even nurses or community health workers) to perform and interpret tests faster
- Offer regular health monitoring, even in remote villages or overcrowded cities
AI solutions in diagnostics can help level the playing field, making advanced healthcare less dependent on geography or local resources.
While there’s still a way to go before everyone benefits equally, even in 2025, remote healthcare powered by AI is changing expectations and raising the bar for what’s possible—no matter where you live.
Ethical, Legal, and Social Impacts of AI in Medical Diagnostics
Ensuring Data Privacy and Security in Healthcare AI
Protecting patient information is one of the most important issues when using AI in healthcare. Medical records hold private details, and the surge in digital health data presents new risks for leaks or hacks. Laws like HIPAA (in the US) and GDPR (in Europe) exist to protect personal information, but AI brings extra complexity. Some newer types of data—like those from wearables or genetic tests—may not always fall under existing safeguards. Security tools help, but nothing beats a layered approach, which can include:
- Encrypting both stored and transmitted data
- Limiting who can access sensitive information
- Regularly testing AI systems for vulnerabilities
Patients have more reason than ever to worry about how their health information is being shared and stored, especially when so many devices and systems are connected.
Addressing Algorithmic Bias and Fairness
AI tools can "inherit" the biases of the data they’re trained on or their programmers. That means they might make more errors for certain groups of people—by gender, race, or age—if those groups are underrepresented or misrepresented. This can lead to unfair treatment or incorrect diagnoses. Steps to promote fairness:
- Review training data sets for diverse representation
- Test AI outcomes on all major patient groups
- Adjust for biases using feedback and updated datasets
| Sample Group | Error Rate with Biased AI (%) | Error Rate with Audited AI (%) |
|---|---|---|
| Group A | 8.5 | 2.1 |
| Group B | 13.2 | 3.4 |
| Group C | 11.8 | 2.9 |
Balancing Automation with Clinical Expertise
While AI speeds up some diagnostic tasks and can spot patterns that humans might miss, it doesn’t replace experienced medical judgment. There’s a real risk if people rely too much on "black box" answers without understanding how the AI came to its decision. For any diagnosis or major care decision, doctors need to stay involved.
- AI should be a tool, not the only voice in the room
- Decisions should blend AI input with clinical know-how
- Ongoing training helps healthcare workers use AI responsibly
Striking a balance between speed and careful review will be a challenge as AI becomes standard in more clinics. The goal is better care, not just faster predictions.
Challenges and Limitations in Implementing AI in Diagnostics
The promise of artificial intelligence in medical diagnostics is hard to ignore, but getting these tools up and running in the real world isn’t as clear-cut as it seems. Many hospitals find themselves held up by practical, technical, and regulatory problems that slow or block progress. Here, we’ll outline some of the main obstacles and explore how they affect healthcare day to day.
Overcoming Integration Barriers in Clinical Settings
AI doesn’t slip unnoticed into the daily routines of busy clinics. Setting up sophisticated diagnostic tools often means changing electronic records, updating process flows, and retraining staff. Healthcare systems deal with issues like:
- Inconsistent data quality: Patient records and imaging files can be missing information, contain errors, or be formatted in old, incompatible systems.
- Staff skepticism: Many people are used to traditional processes and may hesitate to trust software with such high stakes.
- Workflow disruption: Even well-designed AI can slow things down if it’s not tailored to the unique environment of each clinic.
AI isn’t just another app added to the system: hospitals may need to rework how they handle data and train teams, which can take months or even years.
Regulatory Hurdles and Medical Device Approval
Approving AI for medical use isn’t simple. Diagnostic AIs are often considered medical devices, meaning they must be reviewed by regulatory bodies to make sure they’re safe and effective. This process brings its own issues:
| Challenge | Description |
|---|---|
| Regulatory complexity | Multiple agencies with different requirements |
| Changing AI models | Software that evolves can need repeated checks |
| Lack of clear standards | Rules often lag behind technology advances |
It’s tough for developers to predict how regulators will view a newer technology. As emerging technology trends show, businesses face similar hurdles when shifting to new cloud tools or adopting smarter computing systems across sectors, making clarity and adaptation essential.
Quality Assurance and Accountability in AI Systems
It’s one thing for an AI to work well in a controlled lab, but quite another for it to deliver reliable results across millions of real patients in unpredictable conditions. Some key issues:
- AI ‘hallucination’: Sometimes, the system outputs results that simply aren’t true or justified by the data.
- Bias in data: If the training data doesn’t match the real-world population, certain groups may be misdiagnosed more often.
- Difficult accountability: When an AI makes a mistake, it’s still unclear who’s responsible—the developer, the hospital, or the provider?
Hospitals need quality checks and clear procedures to spot errors, plus a chain of accountability if a diagnostic misstep leads to harm.
Adopting AI in diagnostics is not a plug-and-play affair. Bold plans must be backed by practical steps—improving data systems, updating regulatory rules, and making sure everyone from IT staff to physicians is on board with this new way of working.
The Future of AI in Medical Diagnostics and Healthcare Innovation
To be honest, it feels like science fiction is turning into reality right in front of us. AI is going to shape medical diagnostics in ways that reach way beyond what most clinics are doing now. We’re talking about much more than faster test results—this is medicine becoming more tailored, connected, and sometimes, eerily predictive. Let’s see what’s right around the corner.
Integrating Multi-Omics and Genomics for Advanced Diagnostics
Multi-omics combines different layers of information from your body—like genetic data, protein levels, and even your metabolic markers. AI tools are now able to sift through these huge datasets and come up with patterns doctors would have never spotted by hand.
- Genomic sequencing gets even cheaper and more available.
- Smart algorithms help suggest which mutations actually matter for each patient.
- Early disease signals are spotted before anyone feels sick.
| Omics Type | AI Use Case | Benefit |
|---|---|---|
| Genomics | Detecting rare mutations | Faster diagnosis |
| Proteomics | Identifying disease biomarkers | Earlier intervention |
| Metabolomics | Finding metabolic irregularities | Custom treatments |
The mix of real-time data and AI-backed analysis could make medicine feel less like guesswork and more like a custom game plan crafted for every person.
Collaborative Models for AI Development in Healthcare
Building the next wave of medical AI isn’t a one-person job. Hospitals, technology companies, and researchers are starting to work in teams to build smarter, safer tools—that don’t just sit in a lab but actually make a difference in clinics.
- Shared datasets that protect privacy but help improve AI algorithms.
- Open-source tools so smaller health systems can get involved.
- Cross-discipline teams, putting doctors, engineers, and patients in the same room.
These fresh collaborations could be what makes AI trustworthy in the long run—people bring different strengths and make sure solutions work everywhere, not just in well-funded centers.
AI’s Role in Population Health and Preventive Medicine
On a bigger level, AI is about to shake up public health—catching patterns, tracking risks, and even recommending steps for entire communities, not just individuals.
- AI sorts through population-level data to spot outbreak trends or pressing health threats.
- Predictive analytics get used for tracking chronic disease rates and catching early warning signs.
- It helps design more targeted public health campaigns, so resources go where they’re needed.
Emerging technologies are already nudging us closer to a world where AI keeps entire populations healthier by working in the background, long before anyone notices symptoms.
Healthcare’s future will blend smart machines with experienced people, giving us the best shot at solving the toughest medical puzzles—and maybe preventing a few crises before they even start.
Conclusion
So, where does all this leave us? AI is already making a real difference in how doctors spot and treat diseases. It’s not just about fancy machines or complicated algorithms—it’s about helping people get the right care, faster and more accurately. Sure, there are still some bumps in the road. Things like privacy, fairness, and making sure everyone has access still need work. But the progress so far is hard to ignore. As these tools keep getting better, it feels like we’re just at the beginning of what’s possible. In the end, AI isn’t here to replace doctors—it’s here to give them better tools, and maybe even a bit more time to focus on what matters most: the patients. The future of healthcare looks different, and honestly, it’s kind of exciting to see where it goes from here.